The global health crisis reveals that only 32% of pregnant women gain healthy weight gain. A call for optimized standards.

The findings are based on a study led by Monash University and published in the BMJ. Researchers warn that unhealthy weight gain during gestation could cause serious health complications in both mother and baby.(1✔ ✔Trusted Source
Gestational weight gain and risk of adverse maternal and neonatal outcomes in observational data from 1.6 million women: systematic review and meta-analysis
Go to source)
Risks of preterm birth and low birth weight are linked with low GWG. Simultaneously, higher risks of large birth weight, caesarean, hypertensive disorders in pregnancy, and admission to neonatal intensive care are associated with high GWG.
The revelation stress that new global standards and policies are critically needed to curb such pregnancy health crisis.
TOP INSIGHT
Did You Know>
Can #pregnancy #weightgain affect your baby’s health? Low #gestational_weight_gain (GWG) is linked to #preterm_birth and low birth weight; high GWG links to high birth weight & #hypertensive_disorders. Time for clear guidelines! #obstetrics #neonatology #womenshealth #GWG #birthweight
The Global Scale of the Issue: 130 Million Births Affected Annually
Each year 130 million births occur globally in total, in the context of increasingly unhealthy and processed food supply and environmental drivers, causing an epidemic of excess GWG.First author Dr. Rebecca Goldstein, from the Monash Centre for Health Research and Implementation (MCHRI), said the study’s results underlined the need for international action.
“These findings reinforce the need for international reference standards for healthy GWG alongside lifestyle support and public health measures to improve outcomes for mothers and babies worldwide,” Dr. Goldstein said.
Most countries rely on Institute of Medicine GWG guidelines, but these are based on data from predominantly Caucasian women in high income countries in the 1980s, so they don’t reflect ethnically diverse populations across low, middle and high-income settings, or changes in food supply and environment that are driving global trends such as rising weight (BMI).
World Health Organization Initiative and Research Collaboration
In response, the World Health Organization (WHO) has launched an initiative to develop global healthy GWG standards aimed at defining optimal GWG recommendations across diverse settings.To support this initiative, Monash University researchers and collaborators from the WHO analysed data from 40 observational studies involving 1.6 million women aged 18 and over from five of the six WHO defined world regions that reported pregnancy outcomes according to BMI and GWG from 2009 to 2024. Of these 40 studies, 36 were considered to be high quality.
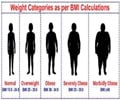
Around half (53 per cent) of study participants had a healthy pre-pregnancy BMI, with others classified as below (6 per cent), above (19 per cent), or well above healthy weight (obese) (22 per cent).
Only a third (32 per cent) had GWG within recommended ranges, with 23 per cent gaining below and 45 per cent gaining above recommended.
Addressing Data Gaps in Low-Income Countries
Based on WHO BMI criteria, the research study found that GWG below the recommended range was associated with: lower risk of caesarean delivery; a large for gestational age infant; and high birth weight (macrosomia) but higher risk of preterm birth; a small for gestational age infant; low birth weight; and respiratory distress.Conversely, GWG above the recommended range was associated with: a higher birth weight and a higher risk of caesarean delivery; hypertensive disorders of pregnancy; a large for gestational age infant (macrosomia), and admission to a neonatal intensive care unit; and a lower risk of preterm birth and a small for gestational age infant.
Similar patterns were apparent when Asian BMI categories were used in studies conducted in this world region.
The researchers point to some limitations, such as variations in BMI and GWG classifications, and note that few studies from low-income countries met their inclusion criteria, limiting diversity. Nor can they rule out the possibility that other unmeasured factors, such as smoking status, age and ethnicity, may have influenced their results.
Improving Health for the Next Generation
Senior author Professor Helena Teede, who is Director of the Monash Centre for Health Research and Implementation, and an Endocrinologist at Monash Health, said the study supported the need for a global approach.“Our findings inform and support the need for optimized, evidence-based WHO international GWG reference standards based on individual patient data, applicable to contemporary and diverse global populations,” Professor Teede said.
“This work builds on and improves current recommendations and highlights the need for multi-level support to improve the health of mothers and babies worldwide.
“Whilst this work supports guidance on healthy GWG, it will need to be incorporated into individualized care to meet the needs of those in pregnancy, limiting stigma and optimizing healthy outcomes for women and the next generation.”
“Ultimately, the burden of health impacts shown here mandate action to support women across policy, healthcare and individual level solutions for the health of mothers and babies.”
Reference:
- Gestational weight gain and risk of adverse maternal and neonatal outcomes in observational data from 1.6 million women: systematic review and meta-analysis - (https://www.bmj.com/content/391/bmj-2025-085710)
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email