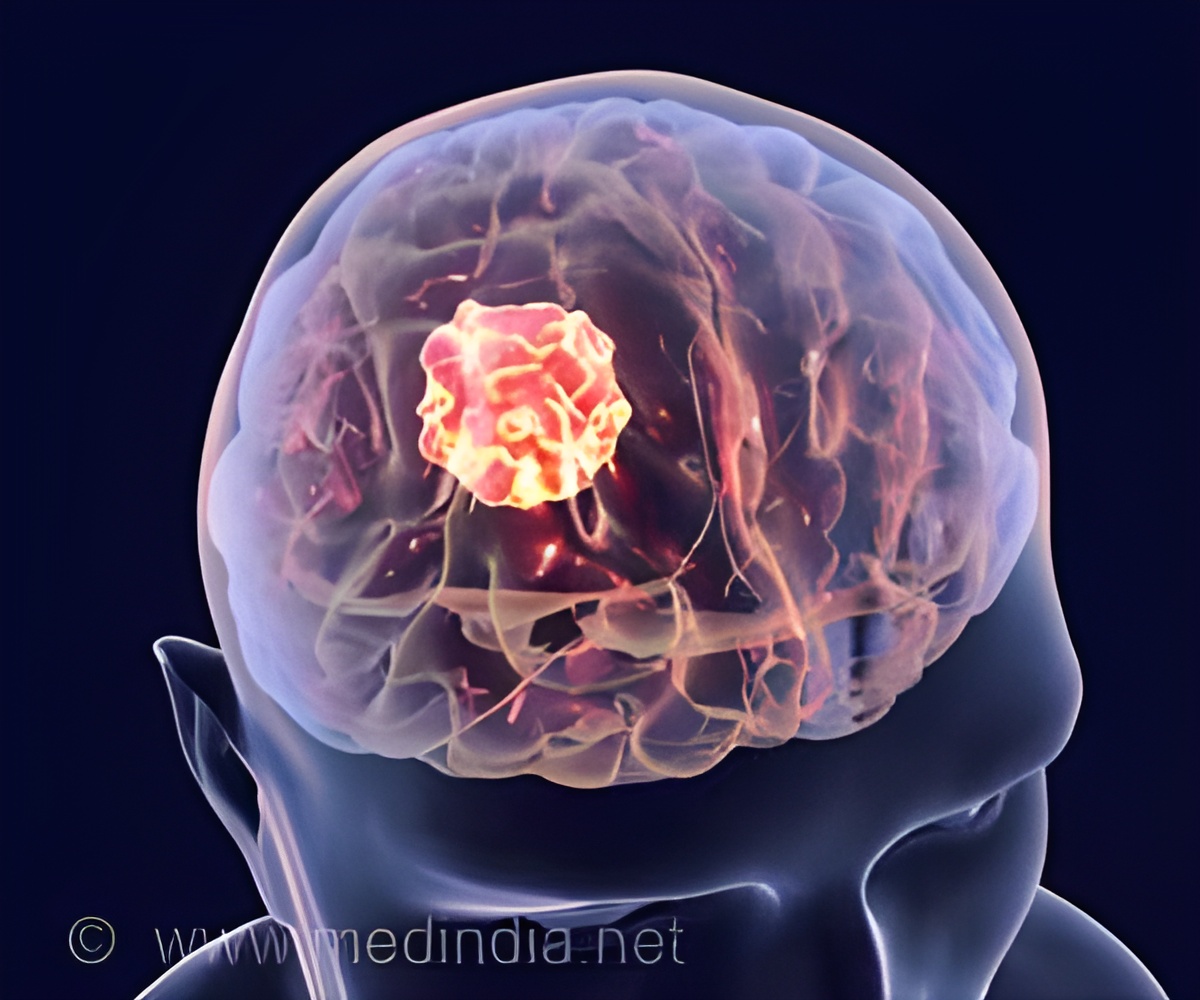
A highly effective approach for taking on glioblastoma has been discovered by scientists.
TOP INSIGHT
Scientists are the first to apply the microshells in a way to bolster the effectiveness of immunotherapy against glioblastoma.
They created hollowed particles, called microshells, made of silica (glass) and filled them with near body-temperature fluorocarbon liquid—a type of highly volatile and inert substance that is FDA-approved as an ultrasound contrast agent. The scientists injected the microshells into glioblastomas in mice and used high intensity focused ultrasound (HIFU) to blow up the shells inside the tumor. The shear force generated by the explosions ruptured the cancer cells to release tumor proteins.
“The silica shells are like micro-sized Christmas tree ornaments,” explained Kummel. “The HIFU ultrasound is like a cat paw that breaks them open. The liquid inside turns to gas when the nanoshells break, thereby rupturing the cancer cells.”
Kummel added that the blast releases tumor proteins which attract white blood cells to the tumor. “When combined with the immunotherapy that is currently approved for patient use, these released proteins train the immune system to combat the tumor,” he said.
Chen, co-author on the paper, agreed. “Without white blood cells inside the tumor, immunotherapy does not work. The trick is to find ways to help the white blood cells get into the tumor.” That trick, according to Chen, involves rupturing the cancer cells at body temperature—something they could do with HIFU—because higher temperatures compromise the effectiveness of white blood cells to fight off the tumor.
Originally, the microshells were developed by UC San Diego’s Professor of Chemistry and Biochemistry William Trogler and Surgical Oncologist Sarah Blair of UC San Diego Health, Moores Cancer Center, for marking breast tumors for surgical removal.
This research was supported by the National Cancer Institute of the National Institutes of Health (T32 Training grant no. 5T32CA153915-08; U54 supplementary grant no. 5U54CA132379-08; 1RON1NS097649-01; 9R44GM128223-02) and funds from the Burroughs Wellcome Fund, the Doris Duke Charitable Foundation, the Sontag Foundation and the Kimmel Foundation.
Source-Newswise
 MEDINDIA
MEDINDIA



 Email
Email