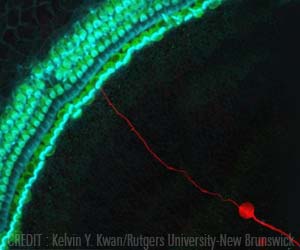
‘Stem cells from the epithelial intestinal lining becomes more active when exposed to glucose.’
Tweet it Now
"For example, can you feed stem cells to make tissues of different sizes and cellular makeup? Can you tell a tissue that’s proliferating when to stop growing?"The ability of the intestinal lining to respond to your food depends on stem cells tucked down in tiny crypts along the epithelium. Certain cues cause stem cells to grow more epithelium, to be able to handle a higher volume of food coming in.
"If I go on vacation and start eating more food, my tissues will grow. But at some point, I’ll come back and my intestinal epithelium will stop growing and shrink back down," Dailey says. "How do the stem cells know to grow it or when to stop? What’s the signal?"
Stem cells are always replacing cells that are lost during normal wear and tear in the intestines. Dailey says most adults’ stem cells are focused on this renewal process, rather than growth, most of the time.
Dailey and a team of researchers looked for signals and cellular responses of intestinal epithelial cells during growth and renewal, and published their findings in the Journal of Cellular Physiology.
Advertisement
The researchers suspected that the availability of glucose might trigger a shift from a renewal mode to a growth mode.
Advertisement
The study showed that stem cells exposed to higher levels of glucose had higher rates of glycolysis, but rates of oxidative phosphorylation didn’t change. In other words, the stem cells switched into a growth mode when exposed to more glucose.
"In the past, a switch from oxidative phosphorylation to glycolysis was thought to be an indication of cancer. Now we know it is just an indication of a cell that’s proliferating. And our team was the first to find it in intestinal epithelial stem cells," Dailey says.
Next, the researchers investigated the driving force behind the switch to glycolysis, focusing on protein kinase networks associated with glucose transport into the cell. They assumed the same networks were operating in both low and high glucose conditions, and that they were more active when exposed to higher levels of glucose.
"Turns out, not the case," Dailey says. "A totally different pathway is used under low and high glucose conditions. The stem cell is able to say, ’I have high glucose and I am going to use different protein kinase networks to get it into the cell.’"
The use of two different protein kinase networks associated with renewal and cell proliferation has implications for cancer research. "If you want to stop cell proliferation by blocking protein kinase networks, you need to know what networks to target. We’ve shown that networks associated with growth are different from renewal," Dailey says.
In addition to its cancer applications, the research provides some basic answers about how stem cells work and paves the way for further research, according to Dailey.
"We were approaching intestinal epithelial stem cells as a model system to ask, ’How can you make tissues of different sizes and cellular makeup? Can you feed stem cells of your kidneys or bone marrow and get different types of tissue? There’s a lot to learn, but we had to start from the beginning," she says.
Source-Eurekalert