Patients with advanced Non-Hodgkin lymphoma who received CAR T cell treatment, and chemotherapy, showed increased treatment efficacy and less toxic side effects.
‘Patients with advanced Non-Hodgkin lymphoma (NHL) who received a Chimeric Antigen Receptor (CAR) T cell treatment, and chemotherapy, showed increased treatment efficacy and less toxic side effects.’





The paper reported the results of the first 32 patients in a dose-finding trial of JCAR014 following a round of chemotherapy, called lymphodepletion, designed to create a more favorable environment for the CAR T cells to grow in the patient's body. Key findings of the study demonstrated the importance of the choice of lymphodepletion regimen and the effects of different doses of CAR T cells.50% of the 18 patients who were evaluable for efficacy after receiving CAR T cells and chemotherapy agents fludarabine and cyclophosphamide (Cy/Flu) had a complete response, which compares favorably to the 8% complete response rate in patients who received JCAR014 plus cyclophosphamide-based chemotherapy without fludarabine. As previously reported, dose-limiting toxicities were observed in some patients in this dose-finding study who received the highest CAR T-cell dose. The study continues with the intermediate CAR T-cell dose.
In patients that received Cy/Flu lymphodepletion and the intermediate dose of JCAR014, the data showed a promising early efficacy and side effect profile. Specifically:
- Overall Response rate: 82% (9/11)
- Complete Response rate: 64% (7/11)
- Severe Cytokine Release Syndrome: 9% (1/11)
- Severe neurotoxicity: 18% (2/11)
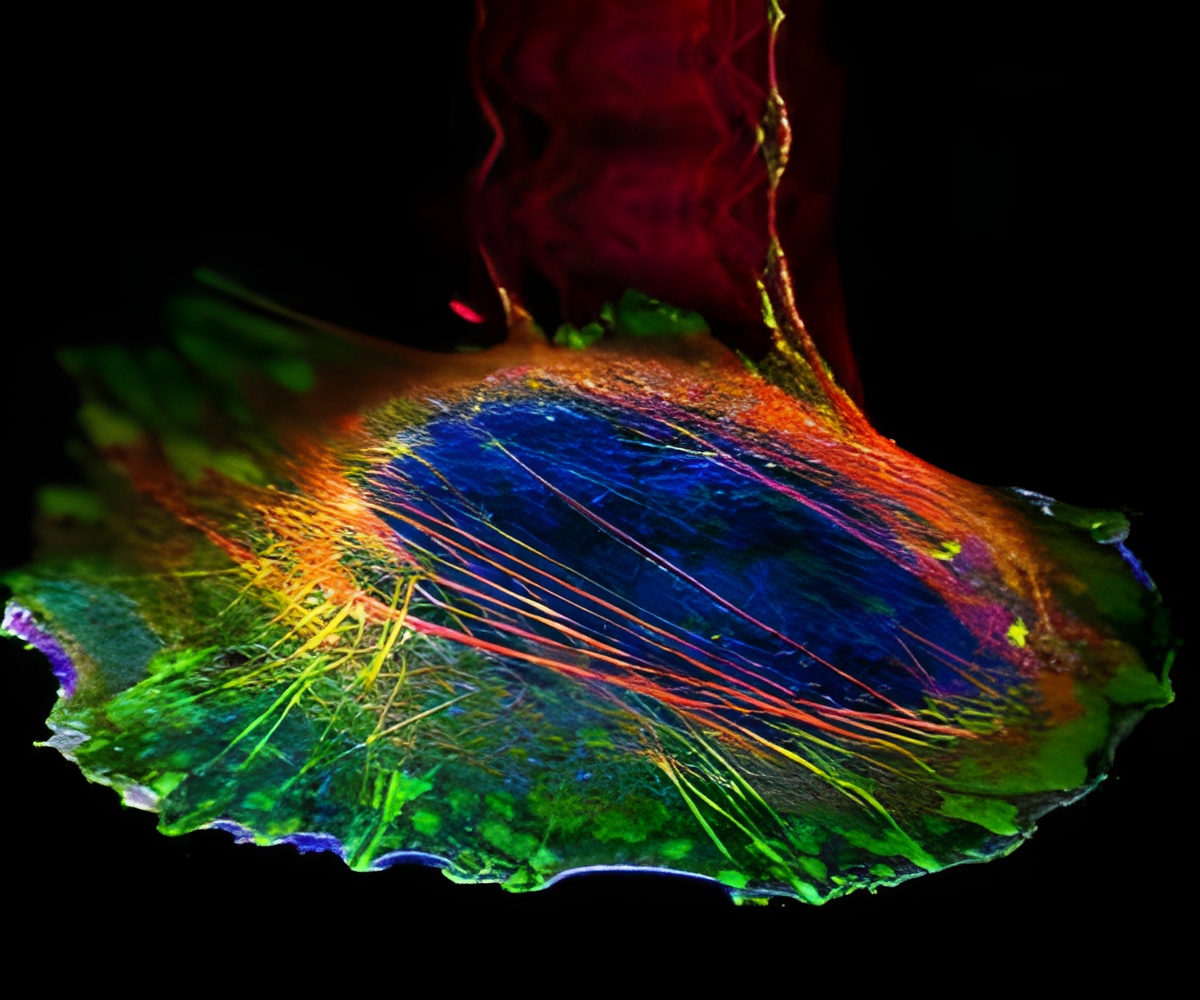
JCAR014's hallmark is its use of a one-to-one ratio of helper (CD4+) and killer (CD8+) CAR T cells, which join forces to kill tumor cells that produce CD19, a molecule found on the surface of many blood cancer cells, including lymphoma and leukemia. By controlling the mixture of T cells that patients receive, the researchers can see relationships between cell doses and patient outcomes that were previously elusive. The data also suggest that with a defined one-to-one composition of cells, efficacy of treatment is increased, while toxic side effects are minimized.
Advertisement
"This study shows that at the right dose of CAR T cells and lymphodepletion, we can achieve very good response rates for NHL patients who have no other treatment options," said Dr. Cameron Turtle, an immunotherapy researcher at Fred Hutch and one of the study leaders.
Advertisement
"We are encouraged by the efficacy and duration of response that we are seeing with defined composition CAR T treatment in patients with lymphoma and other B-cell malignancies," said Mark J. Gilbert, Juno's Chief Medical Officer. "We hope that the insights from JCAR014 will make it possible to bring more life-saving treatments to more patients with blood cancers."
Source-Eurekalert