‘An estimated 10 million people developed tuberculosis (TB) and 1.6 million died of TB globally in 2017, making it the number one cause of death from a single infectious agent. ’
Tweet it Now
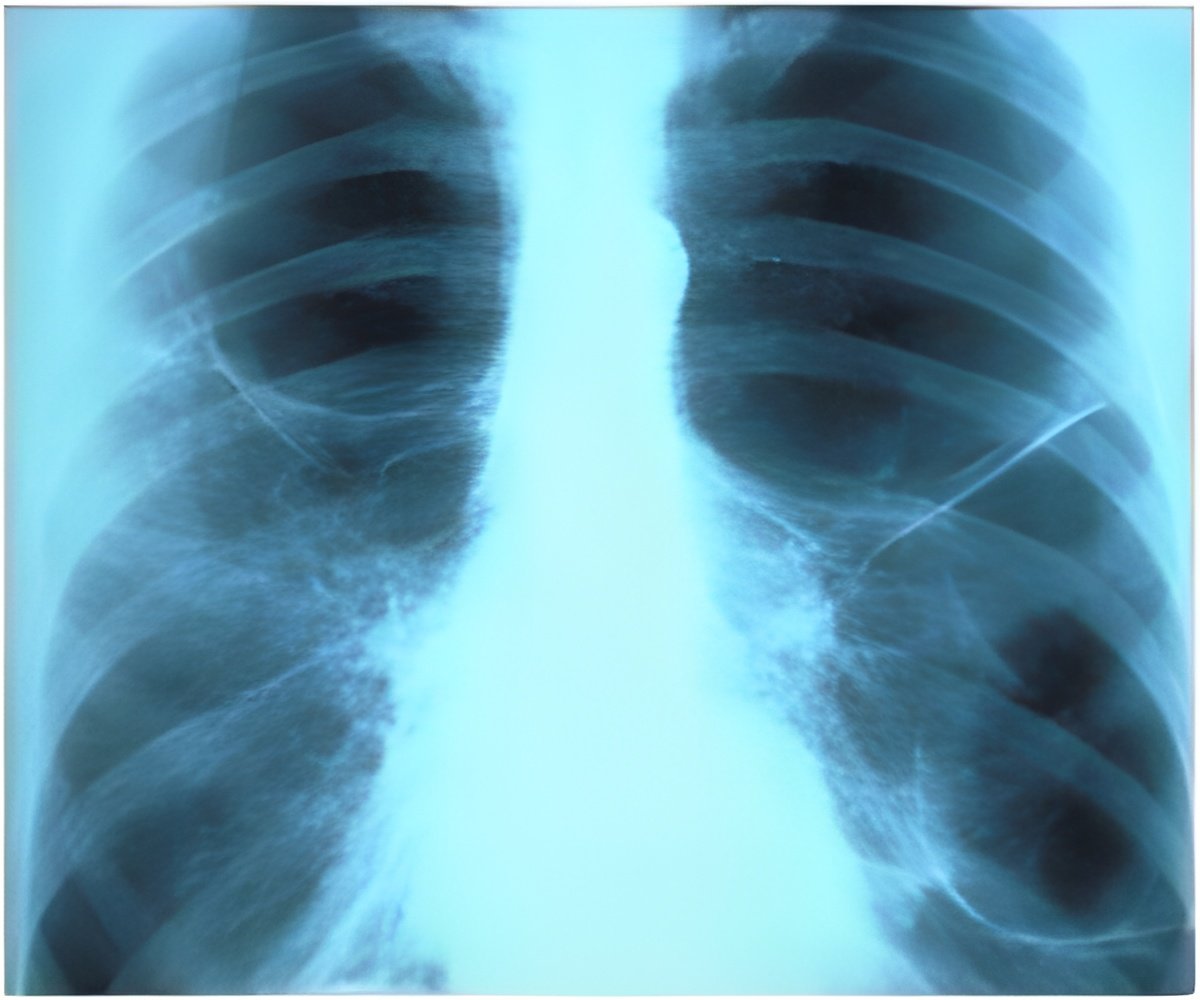
The Special Issue opens with publication of two original research articles: They used data on 329 plasma- and 1,362 tissue-specific drug concentrations from 9 distinct lung lesion types obtained from 15 patients (10 men, 5 women) undergoing lung resection surgery, to develop and evaluate a site-of-action mechanistic pharmacokinetic model for 7 major TB drugs (rifampin [RIF], isoniazid [INH], linezolid [LZD], moxifloxacin [MFX], clofazimine[CFZ], pyrazinamide [PZA], and kanamycin [KAN]). The researchers found that patients receiving standard doses of RIF and INH, who are at the lower range of exposure distribution, spent substantial periods (>12 h/d) below effective concentrations in hard-to-treat lesions, such as caseous lesions and cavities.
Standard doses of INH (300 mg) and KAN (1,000 mg) did not reach therapeutic thresholds in most lesions for a majority of the patient population. The investigators also found that the majority of TB drugs showed poor penetration into the cavitary lesions, leading to inadequate drug levels at the site of disease and increased risk of developing drug resistance.
The authors note that this was a small group of patients from a unique population of TB patients who failed treatment and underwent lung resection surgery. Still, the authors note that the finding that TB drugs do not penetrate equally in different tissues suggests that a patient-focused approach to optimize drug regimen to the disease extent, lesion type, and individual drug-susceptibility profiles may eventually be useful to guide selection of tailored drug regimens with improved outcomes. They provide a web-based tool to further explore this model and results at http: saviclab.org/tb-lesion/.
In the second article, Ankur Gupta-Wright, of London School of Hygiene & Tropical Medicine, and colleagues develop a clinical risk score for identifying HIV-positive patients diagnosed with TB with an increased chance of dying within 2 months. The risk score includes 6 factors that can be measured upon hospital admission, including a urine TB diagnostic test to detect the protein lipoarabinomannan [LAM], age, sex, previous experience on antiretroviral treatment, anaemia, and ability to walk unaided. The score was derived in a cohort of 315 patients from the STAMP TB screening trial in Malawi and South Africa, and externally validated in 644 patients from 2 other studies done in South Africa, Zambia, Zimbabwe, Tanzania, and Kenya. For patients identified by the score as high-risk, the odds of dying within 2 months were about 5 times greater (odds ratio 5.3, 95% confidence interval 2.2-9.5) compared to patients classified as low-risk in the validation cohort. The authors note that this risk score depends on access to urine LAM testing, does not measure all potential predictors of mortality (e.g., TB drug resistance), and further validation in larger and diverse cohorts is necessary. However, this risk score may be able to identify patients who could benefit from enhanced clinical care, follow-up, and/or adjunctive interventions.
Advertisement
The Special Issue will continue with further research and discussion articles appearing over the next several weeks.
Advertisement