Scientists have made star-shaped, biodegradable polymers that can self-assemble into hollow, nanofiber spheres for the first time ever.
Repairing tissue is very difficult and success is extremely limited by a shortage of donor tissue, says Ma, who also has an appointment at the U-M College of Engineering. The procedure gives hope to people with certain types of cartilage injuries for which there aren't good treatments now. It also provides a better alternative to ACI, which is a clinical method of treating cartilage injuries where the patient's own cells are directly injected into the patient's body. The quality of the tissue repair by the ACI technique isn't good because the cells are injected loosely and are not supported by a carrier that simulates the natural environment for the cells, Ma says.
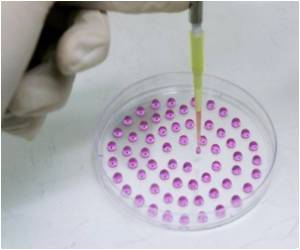
To repair complex or oddly shaped tissue defects, an injectable cell carrier is desirable to achieve accurate fit and to minimize surgery, he says. Ma's lab has been working on a biomimetic strategy to design a cell matrix---a system that copies biology and supports the cells as they grow and form tissue---using biodegradable nanofibers.
Ma says the nanofibrous hollow microspheres are highly porous, which allows nutrients to enter easily, and they mimic the functions of cellular matrix in the body. Additionally, the nanofibers in these hollow microspheres do not generate much degradation byproducts that could hurt the cells, he says.
The nanofibrous hollow spheres are combined with cells and then injected into the wound. When the nanofiber spheres, which are slightly bigger than the cells they carry, degrade at the wound site, the cells they are carrying have already gotten a good start growing because the nanofiber spheres provide an environment in which the cells naturally thrive.
This approach has been more successful than the traditional cell matrix currently used in tissue growth, he says. Until now, there has been no way to make such a matrix injectable so it's not been used to deliver cells to complex-shaped wounds.
 MEDINDIA
MEDINDIA


 Email
Email





