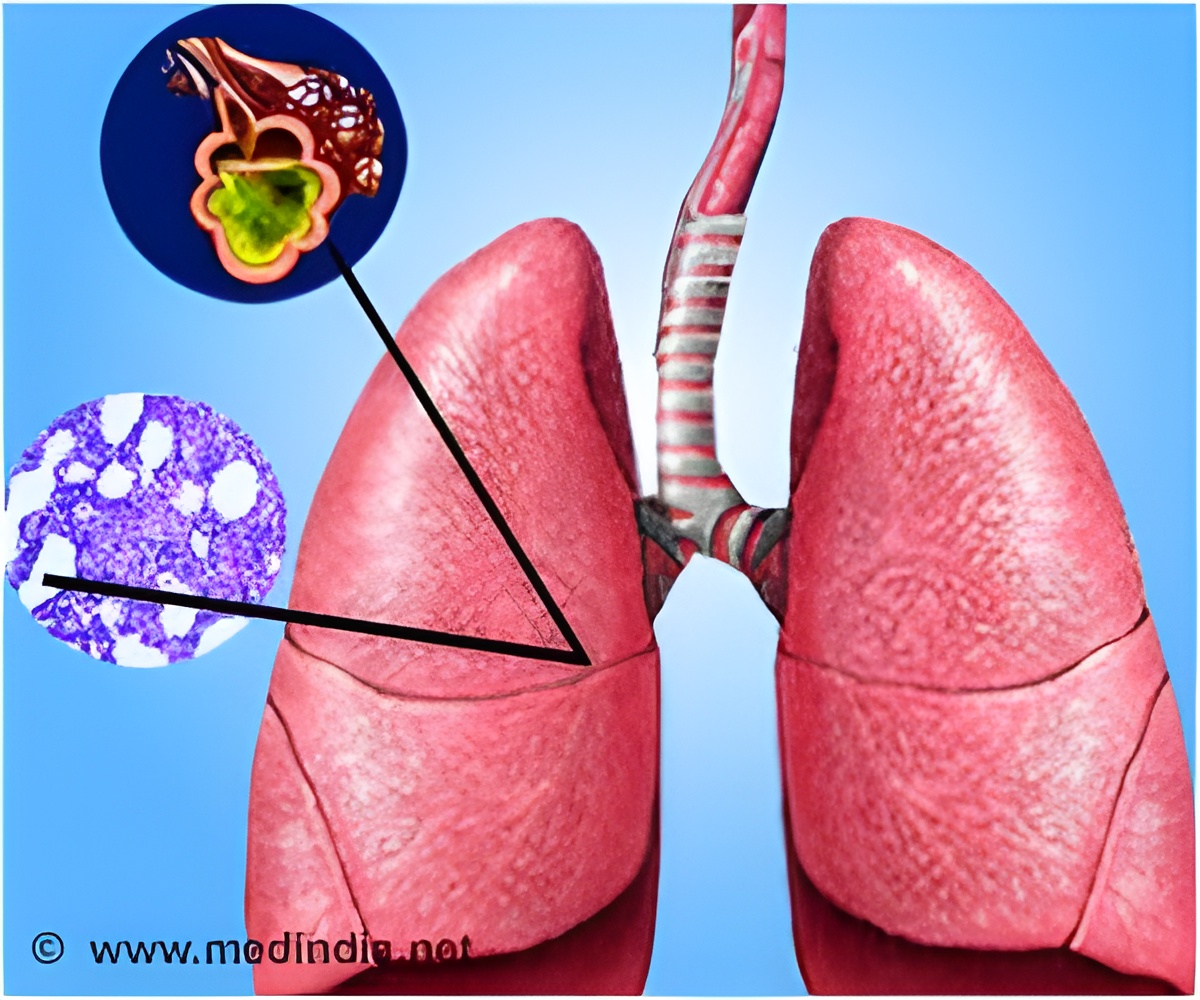
After surgery, acute respiratory distress syndrome is a leading cause of respiratory failure.
The findings are published in the journal Anesthesiology.
"This is a very common reason for needing an extended course of breathing support after surgery, and approximately 20 to 25 percent of patients who develop the syndrome will die from it," says first author Daryl Kor, M.D., a Mayo Clinic anesthesiologist. "It''s well-documented that those who develop this syndrome stay in intensive care longer and in the hospital longer, and the impact of the syndrome can persist for many years."
Prevention of acute respiratory distress syndrome has become a priority for the National Institutes of Health''s National Heart, Lung, and Blood Institute, the researchers noted.
To help prevent the condition, physicians first must identify who is most at risk, and that has proved difficult to do with individual patients, the researchers say. They studied 1,562 surgical patients considered at high risk of developing the syndrome, and found:
* Acute respiratory distress syndrome developed in 117, or 7.5 percent.
*Nine independent factors are predictors of the syndrome: sepsis; high-risk aortic vascular surgery; high-risk cardiac surgery; emergency surgery; cirrhosis; admission to the hospital unit from a location other than home, such as a nursing home or another hospital; increased respiratory rate; and two measurements that indicate hypoxemia, a lower-than-normal oxygen level in the blood.
*Identifying those nine risk factors for surgical patients allowed researchers to refine previous risk prediction models; the new model can be used to identify high-risk patients before surgery for possible participation in acute respiratory distress syndrome prevention studies.
The findings may alter the way patients at high risk of the syndrome are cared for in the operating room, Dr. Kor says.
Future research may include studying the specific role that anesthetic care plays and whether aspects of care in the operating room should be modified in patients at high risk of developing the syndrome, Dr. Kor says.
Study co-authors included physicians and researchers from Mayo Clinic in Rochester and Jacksonville, Fla., and from Beth Israel Deaconess Medical Center, Albert Einstein College of Medicine, University of Texas Southwestern Medical Center, Duke University Medical Center, Massachusetts General Hospital, Wake Forest University Health Sciences, Brigham and Women''s Hospital, University of Michigan School of Medicine and St. Joseph Mercy Hospital. The NIH-funded United States Critical Illness and Injury Trials Group collaborated on the study.
Source-Newswise
 MEDINDIA
MEDINDIA




 Email
Email