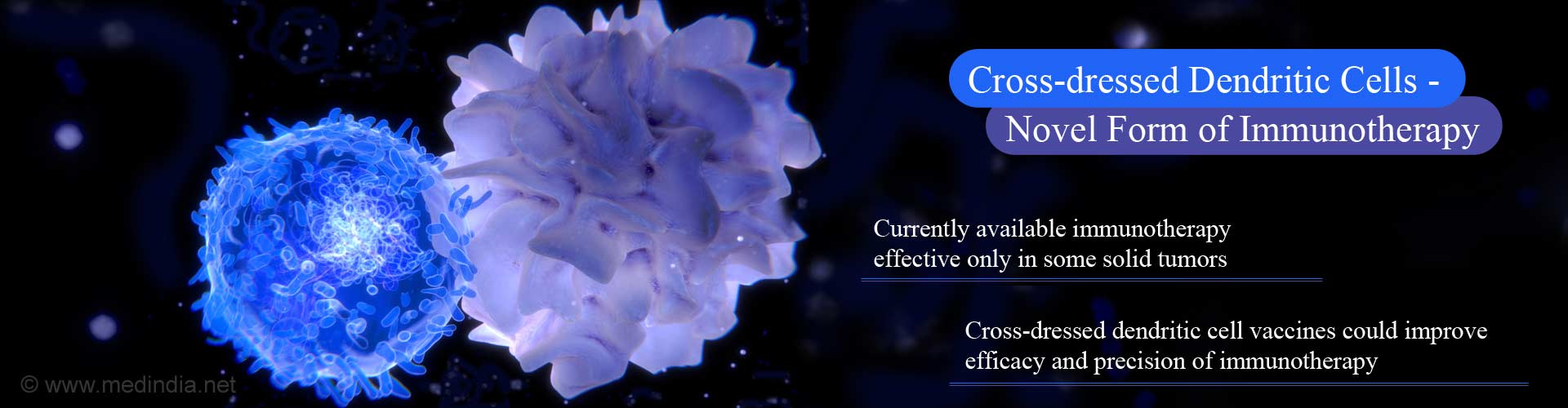
Novel form of immunotherapy where dendritic cells acquire tumor antigens on their surface (cross-dressing) gives boost to cancer treatment options.
Highlights:
- New form of immunotherapy wherein dendritic cells are made to acquire and present tumor antigens on their surface could make immunotherapy more effective and precise
- Immunotherapy, a form of cancer treatment that aims to stimulate the patient’s immune system is currently effective only in some patients with solid tumors.
How Dendritic Cells Acquire Tumor Antigens – EVIR Technology
- Aiming to make immunotherapy more precise and effective in solid tumors, the research team created artificial receptors called EVIRs (extracellular vesicle internalizing receptors) to be incorporated in the dendritic cell vaccine.
- These EVIRs are inserted into the dendritic cells (a type of immune cell).
- These EVIR-incorporated dendritic cells are injected into the patient as a “dendritic cell vaccine”.
- The EVIRs in the dendritic cell are capable of recognizing vesicular structures called exosomes that are released abundantly by patient’s tumor cells. These exosomes carry on their surface various tumor antigens and are also believed to promote tumor growth and metastases.
- The EVIRs efficiently capture the exosomes released by tumor and transfer them on to the surface of dendritic cells, thus facilitating cross-dressing and tumor antigen presentation on the surface of dendritic cells.
- The tumor antigens on the dendritic cells are then presented in a more effective manner to the host T-cells (a type of immune cell) boosting the patient’s immune response to his cancer.
- Imaging techniques have shown that EVIRs aid the direct transfer of tumor antigens from the exosomes to the outer membrane of the dendritic cell.
Older Version of Dendritic Vaccines – Limitations
- Dendritic cells are specialized immune cells capable of capturing antigens from exogenous agents and presenting to the host T cells, which will then attack and destroy the foreign agent.
- To create the dendritic vaccine, dendritic cells removed from the patient, are "force-fed" with tumor antigens, and re-injected back into the patient.
- It was expected that these dendritic cell vaccines would improve the ability of T-cells to destroy the tumor cells that have evolved the art of “hiding” from the immune T-cells of the host.
- Dendritic cell vaccines have attained limited clinical success but do have several limitations; this is because the tumor antigens used to "feed" the dendritic cells are obtained from lab-grown cancer cells and not taken from the patient's tumor.
- These lab grown tumor cells are only partially similar to those of the patient’s tumor cells and thus limit the power of the vaccine because the killer T cells will not be properly stimulated to recognize and kill the tumor cells.
TOP INSIGHT
Displaying tumor antigens on the surface of dendritic cells improves immune destruction of tumor cells by stimulating host T cell immunity against the cancer.
In conclusion, following the promising results of this study, further preclinical trials would still be required before it can be ready to be used on patients. "We are currently exploring potential clinical applications of our technology together with colleagues at the CHUV University Hospital of Lausanne," says De Palma.
Reference:
- Mario Leonardo Squadrito, Chiara Cianciaruso, Sarah K Hansen, Michele De Palma. EVIR: chimeric receptors that enhance dendritic cell cross-dressing with tumor antigens. Nature Methods, (2018); DOI: 10.1038/nmeth.4579
Source-Medindia
 MEDINDIA
MEDINDIA


 Email
Email