A close link between vortex flow and pressure differences in the ventricles, or lower chambers, of the heart has been discovered.
‘The close relationship of vortex and intraventricular pressure difference and showed that both of them can become new markers of the left ventricular relaxation property. ’





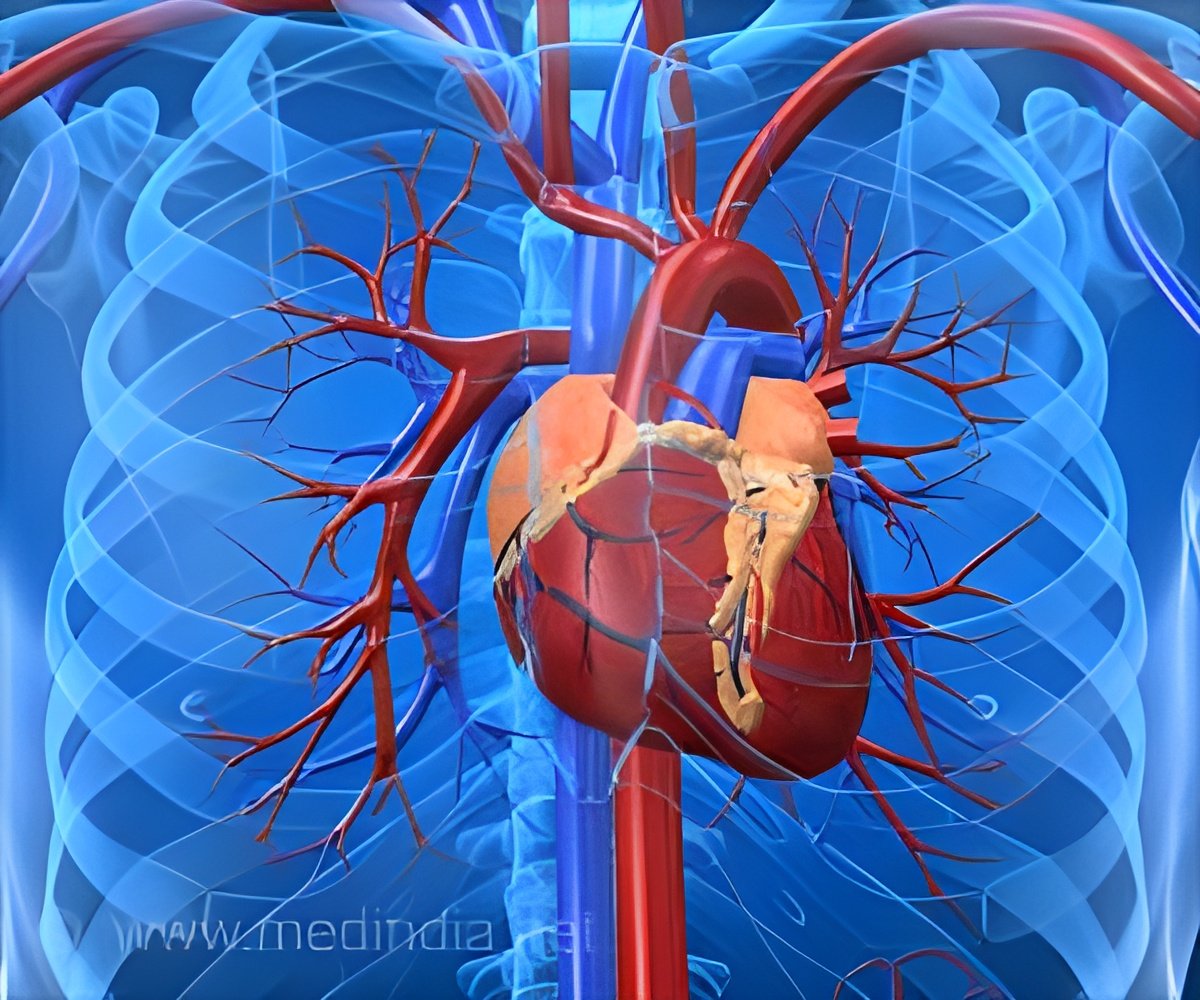
Every beat of the heart consists of two stages. In the first stage, known as diastole, the left and right lower chambers of the heart (called ventricles) relax and expand, and blood flows into them from the left and right upper chambers (called atrium). Once the ventricles are full of blood, the second stage, known as systole, is triggered. The muscles in the ventricle walls contract and blood is pumped from the left ventricle to the aorta (main artery carrying oxygenated blood to the body), and from the right ventricle to the pulmonary artery (carrying deoxygenated blood back to the lungs). Diastolic dysfunction is a common heart condition in both domestic animals and humans, particularly among the elderly, where the diastole stage does not function as efficiently as it should. The muscles in the ventricle walls become thickened and stiff, losing their elasticity, and do not relax and expand properly. As a result, the capacity of these chambers to fill up with blood is reduced. This in turn causes blood to accumulate in other areas of the body.
The restriction in flow causes pressure inside the ventricles to build up as blood pumped with the next heartbeat tries to enter the chamber which, due to its inability to expand properly, lacks sufficient capacity to accommodate it all. Diastolic dysfunction is characterized by an increased pressure in the left ventricle as the oxygenated blood returning from the lungs tries to enter. As the surplus blood has to go somewhere, it also causes blood and pressure to build up in the blood vessels around the lungs (pulmonary congestion) or in the vessels returning blood back to the heart (systemic congestion).
In the case of pulmonary congestion, fluid can leak through the vessel membranes into the alveoli (tiny air sacs that allows air exchange) in the lungs, resulting in pulmonary edema -- a condition where oxygenation of the blood is impaired, leading to breathing difficulties and, in severe cases, to potentially fatal diastolic heart failure.
As blood flows from the left atrium into the left ventricle, it forms a swirling mass of fluid known as a vortex ring. In terms of its fluid dynamics, a rotating vortex is believed to flow more efficiently than a straight, steady flow of fluid and therefore assists filling of the left ventricle during diastole. A healthy heart that exerts sufficient suction force typically has a large intraventricular pressure difference, whereas a heart with diastolic dysfunction has a low intraventricular pressure difference.
Advertisement
For this study, the researchers monitored six healthy anesthetized dogs to determine whether intraventricular fluid dynamics can be assessed clinically using non-invasive imaging techniques, and whether impaired fluid dynamics may be a source of diastolic dysfunction that can lead to heart failure.
Advertisement
Source-Eurekalert