Exposure to chemotherapy drugs is hazardous to health care workers, however, many of them do not use recommended personal protective equipment when handling chemotherapy.

TOP INSIGHT
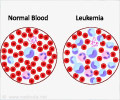
Exposure to chemotherapy by the healthcare workers leads to a range of health issues such as reproductive problems, rare types of cancers and various respiratory and skin conditions.
Exposure to chemotherapy occurs when health care workers inhale vapors or touch contaminated surfaces. Studies have found that nurses who reported handling hazardous drugs had twice the risk of reproductive problems. Other studies report incidences of rare cancers and various respiratory and skin conditions resulting from exposure.
"This is an invisible threat," Friese says. "It's unlike the needle stick where you know when you've been stuck by a needle. Early on we could understand that a needle stick conveyed serious health risks. With chemotherapy exposure, we don't have that smoking gun. This is a subtle threat, but it's a daily threat."
Guidelines from professional societies recommend protective gear including double gloves, eye protection and respirators. These were built into the intervention Friese and colleagues developed. It was a randomized trial including 396 nurses from 12 ambulatory cancer programs. In one arm, nurses received one-hour educational modules about personal protective equipment with tailored messaging addressing their reported barriers to use. They also were asked to report chemotherapy drugs spills and submit plasma samples for analysis. The control arm had only the educational modules.
After two years of the program, the researchers found little difference in the use of personal protection equipment between the two groups and no change over the course of the study. Results are published in Oncology Nursing Forum.
Something must change, Friese says. Health care workers continue to report exposure hazardous drugs. An earlier study by Friese found nearly 17 percent of nurses who work in outpatient chemotherapy infusion centers said they had been exposed to chemotherapy on their skin or eyes.
The researchers propose three ways to start moving the needle on the issue:
1. Engage health system leadership to have a dialogue with staff about personal protection for those who handle hazardous drugs.
2. Develop better personal protective equipment that is easy to use, affordable and protective against hazardous drug exposure.
3. Collect data through a registry to identify and track the health risks from exposure.
Friese uses the analogy of the airplane safety rule to put on your own mask before helping others.
"We need to really anchor that into our community," he says. "Unless you take good care of yourself, you can't be there to take good care of your patient."
Source-Eurekalert
 MEDINDIA
MEDINDIA



 Email
Email