Patients with operable kidney cancers were more likely to have a partial nephrectomy -the recommended treatment for localized tumors- when treated in hospitals that were early adopters of robotic surgery, suggests a new study.
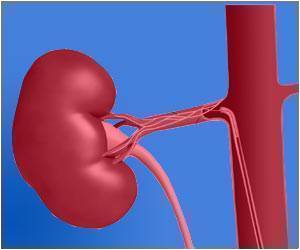
Partial nephrectomy, the removal of a section of the kidney as opposed to the removal of the entire organ, is preferred over total nephrectomy because it can achieve similar outcomes in cancer while avoiding the long-term risks associated with total kidney removal, such as cardiovascular disease, chronic kidney failure and premature death.
"Our study is the first to show, at the hospital level, that more institutional experience with robotic surgery is likely to have resulted in this increase in partial nephrectomy," said the study's lead author, Ganesh Sivarajan, MD, a post-doctoral fellow in the Department of Urology at NYU Langone. Hospitals that had not adopted robotics by 2008 performed partial nephrectomies in only 20% of cases.
For their study, the research team analyzed retrospective data on all nephrectomies from all payers from seven states (Arizona, Florida, Maryland, North Carolina, New York, New Jersey, and Washington) to extract data on 21,569 kidney cancer surgeries. They then sorted these procedures by hospital, and associated their frequency with the timing of each hospital's acquisition of surgical robotics.
Danil V. Makarov, MD, MHS, the study's senior author, and Director of Urological Health Services Research at NYU Langone, said: "Robotic surgery was not originally designed for treatment of kidney tumors, but what we see here is a case of reinvention, or adaptation. In this case, the reinvention has served to provide patients increased access to an underutilized, guideline-supported procedure."
Robotics offers other important advantages over laparoscopic and open surgery, according to Dr. Sivarajan. "It has outstanding magnification and permits improved manual dexterity," he said.
"We strongly believe that our analysis offers significant public health implications for the delivery of guideline-based care for kidney cancer," Dr. Makarov said. "As we move toward expanded use of cost effectiveness data, we need to leave room for this sort of evolution."
 MEDINDIA
MEDINDIA


 Email
Email










