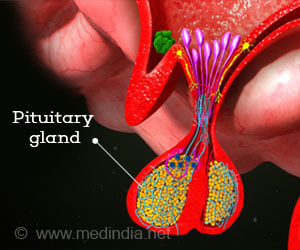
Hypopituitarism, or pituitary insufficiency, occurs when the pituitary gland does not produce sufficient amounts of hormones.

TOP INSIGHT
The pituitary gland is often called the master gland because the hormones it produces impact many bodily functions.
The rare disorder can occur due to abnormal development or later in life as a result of a tumor, traumatic brain injury, hemorrhage or autoimmune condition, according to the Society's Endocrine Facts and Figures Report. Hypopituitarism affects about 45 people in every 100,000, according to the guideline.
"Hypopituitarism can manifest as low levels of a variety of hormones, including cortisol, thyroid hormone, estrogen, testosterone and growth hormone," said Maria Fleseriu, MD, FACE, of Oregon Health & Science University in Portland, OR. Fleseriu chaired the task force that developed the guideline. "The goal of treatment should be to restore hormone levels as close to healthy levels as possible The interactions between these hormones also are very important, and patients might require dose changes of one or more of the replacement hormones after starting or discontinuing another one."
In recommending treatment options, the guideline task force followed the overriding principle of using hormone replacement therapy dose size and timing to mimic the body's natural functioning as closely as possible.
Accurate and reliable measurements of hormones play a central role in diagnosing hypopituitarism and monitoring the effectiveness of treatments, Fleseriu said. Healthcare providers need to keep in mind technical considerations to ensure the testing procedure is as accurate as possible.
Recommendations from the guideline include:
People who have central hypothyroidism should be treated with levothyroxine in doses sufficient to raise levels of the thyroid hormone free thyroxine to the upper half of the reference range. Growth hormone stimulation testing should be used to diagnose patients with suspected growth hormone deficiency.
People who have proven cases of growth hormone deficiency and no contraindications should be offered growth hormone replacement as a treatment option. Premenopausal women who have central hypogonadism, a condition where the sex glands produce minimal amounts or no hormones, can undergo hormone treatment, provided there are no contraindications.
People producing abnormally large volumes of dilute urine should be tested for central diabetes insipidus--a rare condition that leads to frequent urination--by analyzing the concentration of their blood and urine. For patients who have low levels of glucocorticoid hormones, hydrocortisone can be given in a daily single or divided dose.
All hypopituitarism patients should be instructed to obtain an emergency card, bracelet or necklace warning about the possibility of adrenal insufficiency. Patients who are suspected of having an adrenal crisis due to secondary adrenal insufficiency should receive an immediate injection of 50 to 100 milligrams of hydrocortisone.
People who have central adrenal insufficiency should receive the lowest tolerable dose of hydrocortisone replacement on a long-term basis to reduce the risk of metabolic and cardiovascular disease.
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email