Under high glucose conditions, the efficacy of various chemotherapies was significantly enhanced when compared to low glucose conditions.
Increased glucose availability sensitizes pancreatic cancer to chemotherapy
Go to source).
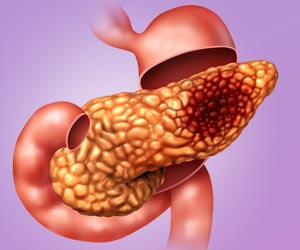
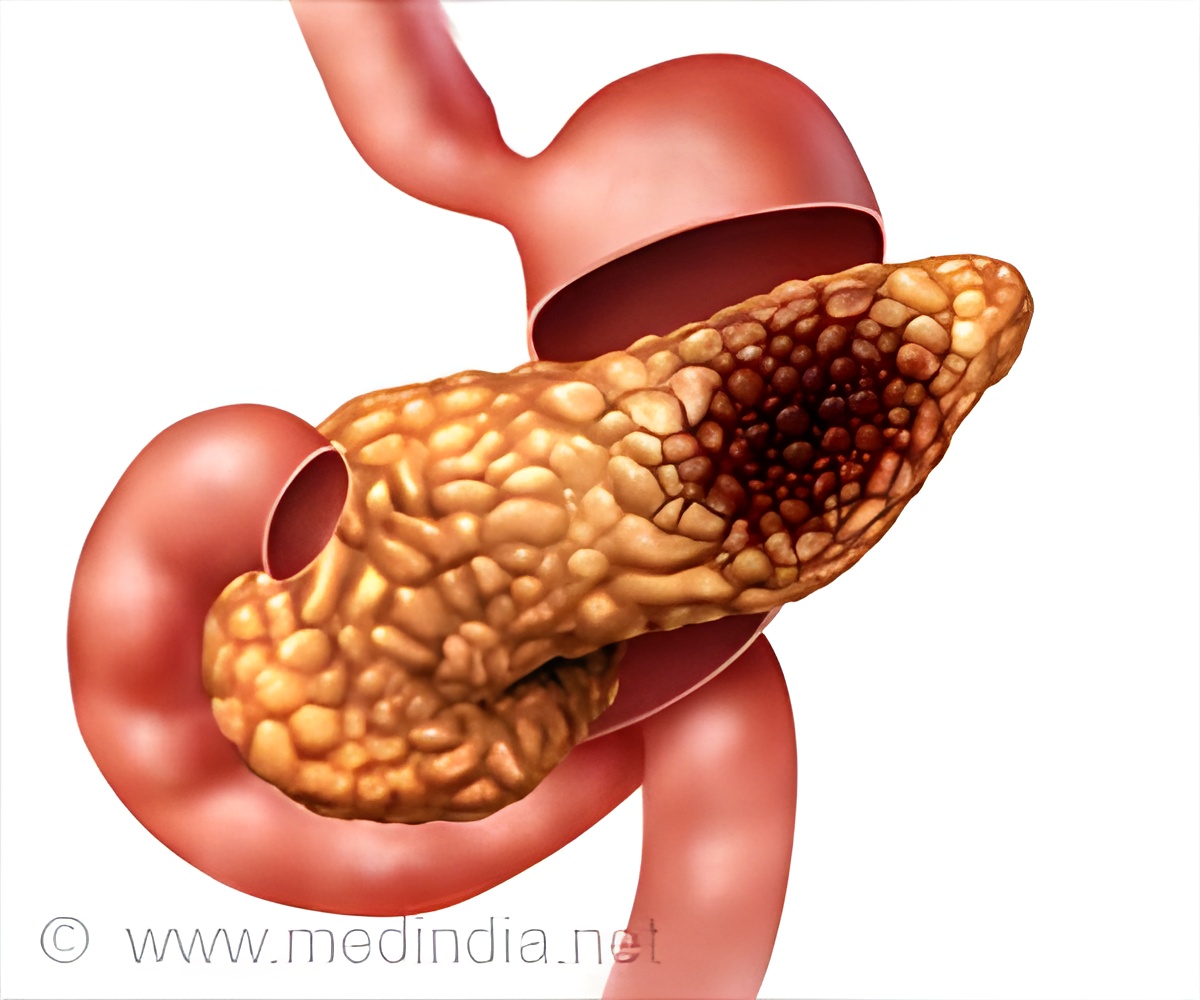
Challenges in Pancreatic Cancer Treatment
Pancreatic cancer is one of the most difficult cancers to treat, being highly resistant to chemotherapy. Although there are fewer than roughly 60,000 new cases of pancreatic cancer diagnosed annually in the U.S., about 95 percent of people with it die from it, mainly because it often goes undetected in early stages. Approved multi-agent chemotherapy regimens offer a marginal advance over single-agent treatments, and resistance to these “cocktails” virtually always develops. Multi-agent chemo offers a median survival benefit of roughly four months over a single-agent. Overall, median survival of patients with metastatic pancreatic cancer in the modern era is just eight to 11 months, and the five-year survival rate is around 3 percent.‘The induction of forced hyperglycemia as a means to sensitize tumors to chemotherapy presents a groundbreaking therapeutic approach for pancreatic cancer. #cancertreatment #cancerofthepancreas ’





These findings present a potentially new method of making chemotherapy more effective against pancreatic cancer, according to the paper’s senior author Jordan Winter, MD, Director Surgical Services, University Hospitals Seidman Cancer Center, John and Peggy Garson Family Endowed Chair in Pancreatic Cancer research and Jerome A. and Joy Weinberger Family Master Clinician in Surgical Oncology.
Promising Approach for Pancreatic Cancer Treatment
“Our findings reveal an approach that would have relatively low-cost and could be easily tested in patients with pancreatic cancer,” said Dr. Winter. Over the past three decades, pancreatic cancer researchers have yet to find new effective targeted therapies. However, if relatively simple interventions can be administered that can greatly enhance the effect of conventional drugs, then patients stand to benefit. Importantly, this advance would potentially bypass the usual cost and time required to develop new therapeutics. This could save over a decade of time and more than $1 billion, based on drug development data.In the study, the researchers validated a prior clinical study by the same authors that showed patients with localized pancreatic cancer and elevated glucose levels were more responsive to chemotherapy. For the current study, the researchers examined the impact of glycemic status on another group of patients treated for metastatic pancreatic cancer. About 33 percent of the patients had elevated glucose levels (at least one glucose reading above 200 mg/dL). There were no appreciated demographic differences between normal (99 mg/dL or lower) and high glucose patients. A greater proportion of patients in the high glucose group had a documented diagnosis of diabetes.
The median overall survival among all patients who completed at least two cycles of chemotherapy was approximately 9.8 months in all the patients, on par with historical clinical trial data. Further analysis showed, however, that patients in the high glucose level group had a nearly 40% lower risk of dying, despite a higher level of a cancer antigen (CA19-9, which is a measure of disease burden), as compared to patients in the normal glucose group.
“Notably, no associated survival difference was observed based on glucose levels in an independent cohort of metastatic patients who did not receive treatment, suggesting that the interaction with glycemic status may be present only for patients who receive chemotherapy,” said lead author Ali Vaziri-Gohar, PhD, of the Case Comprehensive Cancer Center at Case Western Reserve University at the time of the study and now with the Stritch School of Medicine, Loyola University Chicago.
Paired with prior cell culture and clinical data, these clinical data indicated that a high-glucose state could sensitize PDAC to conventional chemotherapy.
Advertisement
In experiments with grafted PDAC tumors on hyperglycemic mice, the researchers found greater sensitivity to single-agent chemotherapy in the two independent models of mice with hyperglycemia. As observed previously with patients in the absence of chemotherapy, no significant differences in growth rates were observed with hyperglycemia compared to mice with normal blood sugar levels in the absence of chemotherapy exposure. The researchers also tested a multiple agent chemotherapy to replicate what a patient might receive today and validated that hyperglycemia alters the metabolic state within tumors to sensitize it to treatment.
Advertisement
In theory, glucose levels can even be modified more precisely through intravenous dextrose infusions (combined with rigorous inpatient glucose monitoring) at the time of chemotherapy administration.” The next step is to implement a clinical trial. Dr. Winter notes that “our patients need better treatment options urgently. Therefore, we are already getting to work designing a trial to treat patients safely with intentionally elevated blood sugars, and will determine if this strategy can improve patient outcomes.”
Reference:
- Increased glucose availability sensitizes pancreatic cancer to chemotherapy - (https://www.nature.com/articles/s41467-023-38921-8)