- Calcinosis - (http://www.sclero.org/scleroderma/symptoms/skin/calcinosis.html)
- Calcinosis Cutis - (http://www.dermnetnz.org/topics/calcinosis-cutis/)
- Shinjo SK, Carlos de Souza FH. Update on the treatment of calcinosis in dermatomyositis. Rev. Bras. Reumatol. vol.53 no.2 São Paulo Mar./Apr. 2013 - (http://dx.doi.org/10.1590/S0482-50042013000200009)
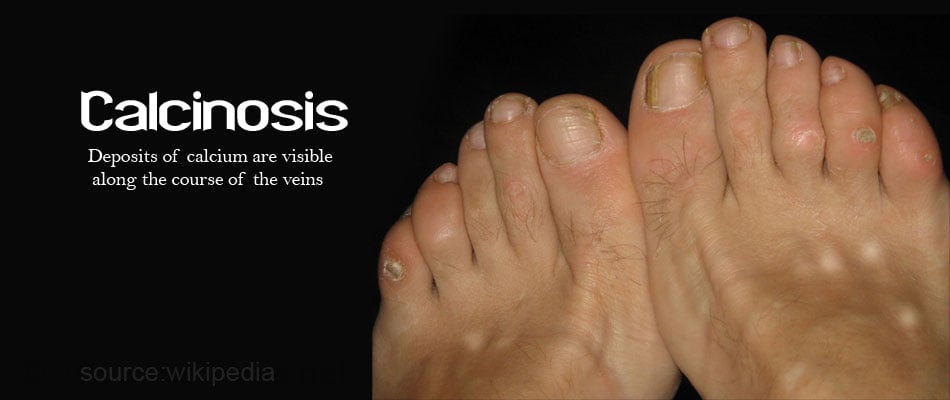
What is Calcinosis?
Calcinosis refers to abnormal deposits of calcium phosphate or hydroxyapatite in the fingers, skin, muscle or other areas of the body as hard lumps or snow balls.
Calcium deposits occur most commonly in the skin and are called calcinosis cutis.
What are the Types of Calcinosis?
There are four types of calcinosis:
Dystrophic Calcinosis:
This is the most common type of calcinosis. The calcium and phosphate levels in the blood are usually normal. It usually affects inflamed, cancerous or necrotic tissues that are damaged due to mechanical, chemical, infectious and other causes.
Metastatic Calcinosis
Metastatic calcinosis, also called as tumoral calcinosis or lipocalcinogranulomatosis, is associated with high calcium and phosphate levels in the blood. Around a third of the conditions that cause metastatic calcinosis have been noted to have an autosomal dominant or autosomal recessive inheritance. The tissues around joints like the shoulders, hips and ankles are usually affected.
Idiopathic Calcinosis
Idiopathic calcinosis occurs in the absence of any tissue injury or systemic metabolic defect. The calcinosis is usually localized to one particular area.
Iatrogenic Calcinosis
Iatrogenic calcinosis occurs secondary to treatment like replacement of calcium or phosphate. Iatrogenic calcinosis may also occur following diagnostic tests. For example, calcium deposits occur in the heels of newborns due to repeated heel sticks.
What are the Causes of Calcinosis?
Causes of calcinosis include:
- Trauma
- Varicose veins
- Infections
- Skin tumors like basal cell carcinoma and pilomatrixoma (benign appendageal tumor)
- Connective tissue diseases like dermatomyositis (skin inflammation), systemic sclerosis (connective tissue disease), cutaneous lupus erythematous (autoimmune disease) and sarcoidosis (inflammatory disease). Calcinosis is a part of CREST syndrome (calcinosis, Raynaud’s disease (rare disorder of blood vessels), esophageal dysmotility, sclerodactyly (localized thickening and tightness of the skin), telangiectasias (spider veins) ). Inherited connective tissue disorders like Ehlers-Danlos syndrome (genetic connective tissue disorders), Werner’s syndrome (adult progeria), Pseudoxanthoma elasticum (progressive calcification) and Rothmund Thomson syndrome can also cause calcinosis
- Panniculitis, which is characterized by inflammation of the fat tissue under the skin
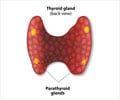
- Primary or secondary hyperparathyroidism: In hyperparathyroidism, calcium crystals usually deposit in the kidney tissue and the condition is called as nephrocalcinosis.
- Paraneoplastic hypercalcemia, where high calcium levels result due to a cancer
- Destructive bone disease like Paget’s disease
- Milk–alkali syndrome, which occurs due to intake of high quantities of calcium and absorbable alkali
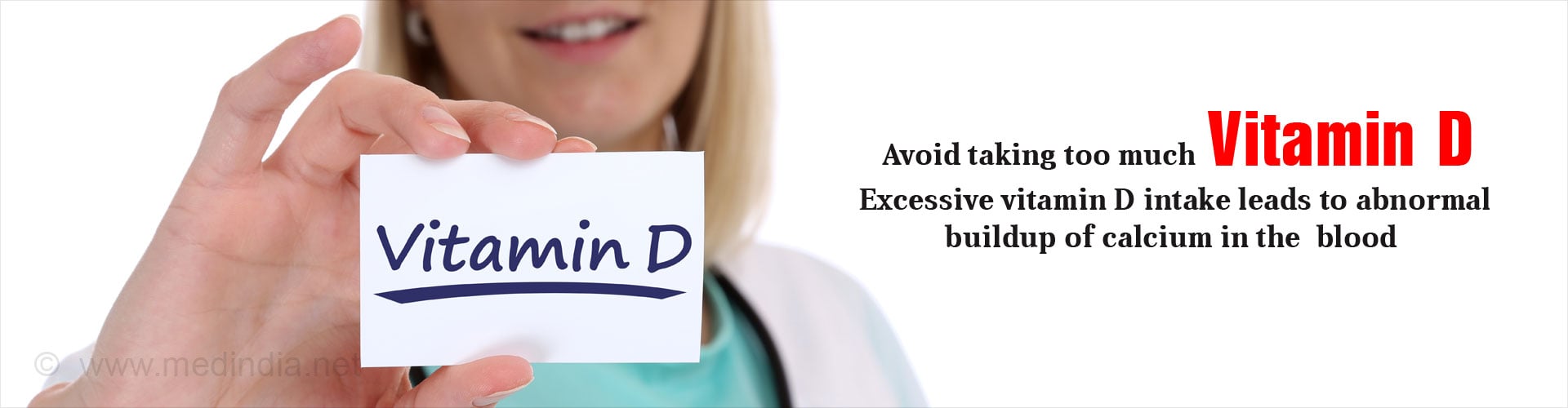
- Excessive vitamin D intake
- Chronic Renal Failure: Patients with chronic kidney failure have high parathyroid hormone and phosphate levels
- Calciphylaxis is a syndrome of calcification of blood vessels, thrombosis or clot formation in blood vessels, and skin necrosis. It is often a consequence of chronic kidney disease
- Acne

What are the Symptoms of Calcinosis?
The symptoms of calcinosis vary depending on the location of the lesions.
- Lesions develop gradually and are usually symptomless
- The skin may be itchy and red
- Some lesions may form ulcers and give out a chalky white discharge
- If the deposit of calcium occurs in the brain, it may manifest with progressive cognitive impairment, mood swings and occasional psychosis
- Gradual thickening of the skin of the face may be noted
- Calcium deposits in joints may damage the joints resulting in pain and disability
- Symptoms of the underlying condition like connective tissue disorder, kidney failure or tumor may be noted
How Do You Diagnose Calcinosis?
Diagnosis is made based on few laboratory tests and radiological tests
Laboratory Tests
Blood tests are done to test for the following parameters:
Serum Calcium Levels: The serum calcium levels may be higher or lower than normal.
Hypercalcemia – If the calcium levels are found to be higher than the normal, the following conditions could be the cause of calcinosis:
- Milk-alkali syndrome (high blood calcium caused by taking too much calcium)
- Familial hypocalciuric hypercalcemia (mutations in the calcium-sensing receptor gene (CASR))
- Dystrophic calcinosis (skin condition characterized by calcification of the skin)
Hypocalcaemia - If the calcium levels are found lower than the normal, the causes of calcinosis could be:
- Pseudohypoparathyroidism (resistance to parathyroid hormone)
- Osteomalacia (softening of the bones)
Serum Phosphorus Levels: The serum phosphate levels may be higher or lower than normal.
- Hyperphosphataemia - If high levels of phosphorus are found in the blood, it is important to rule out metastatic calcinosis or rule out the conditions causing metastatic calcinosis like calciphylaxis and sarcoidosis
- Hypophosphatemia - If lower than normal phosphorus levels are found in the blood, then causes of dystrophic calcinosis like tumors or infections need to be ruled out
Serum Vitamin D Levels
If the history suggests that the patient is on vitamin D replacement, it is important to check vitamin D levels to rule out high vitamin D levels that may be responsible for iatrogenic calcinosis
Radiological Tests
- X-ray of the extremities helps to locate the deposits
- CT scan of the chest and brain is used to detect any calcium deposits in the chest and brain, to know the extent of the tissue calcification and to rule out any neoplastic or paraneoplastic causes

Tissue Biopsy of the Lesion
The area to be biopsied is infiltrated with a local anesthetic and tissue is biopsied from the lesion. The procedure can be done on an outpatient basis. Calcium deposits are noted in the calcinosis lesions.
How Do You Treat Calcinosis?
The treatment of calcinosis involves treating the lesions as well as the underlying cause:
Treatment of the underlying cause involves:
- Management of trauma
- Blocking contraction of blood vessels by preventing cold exposure and stress, increasing dilatation of blood vessels through heat massage in Raynaud’s disease
- Restriction of calcium and phosphorus intake
- Control of infections by giving prompt and early antibiotic therapy

Pharmacological Treatment:
Medications used to treat calcinosis include the following:
- Colchicine – An anti-inflammatory drug to prevent pain and inflammation
- Diltiazem – A calcium channel blocker to prevent the influx of calcium into cells
- Corticosteroids – To reduce inflammation
- Bisphosphonates – To prevent osteoporosis and bone diseases
- Magnesium and Aluminum Containing Antacids – To prevent hypercalcemia
Surgical Treatment
Surgical treatment is indicated when the lesions become very painful, or ulcerate and recurrent infections occur, or if they cause functional difficulty.
Extra corporeal shock wave therapy is done for chronic resistant calcinosis cutis associated with systemic sclerosis.
Surgical treatment is usually associated with recurrence and the trauma may stimulate further calcification; hence, a small bit is excised before taking a larger incision.
Tips to Reduce Inflammation Associated with Calcinosis
- Close monitoring of calcium and phosphorus levels especially in patients with chronic renal failure is very important
- Proper correction of vitamin D and checking the levels frequently during correction is important to prevent over correction
- Avoid trauma
- Don’t ignore symptoms like psychosis or fluctuating emotions which may be associated with calcium deposits in the brain
 MEDINDIA
MEDINDIA
 Email
Email