- Aspergillus - (https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/aspergillus)
- Aspergillosis - (http://www.mayoclinic.org/diseases-conditions/aspergillosis/basics/tests-diagnosis/con-20030330)
- Treatment for Aspergillosis - (http://www.cdc.gov/fungal/diseases/aspergillosis/treatment.html)
- Diagnosis of Invasive Aspergillosis by Galactomannan Antigenemia Detection using an enzyme immunoassay - (http://antimicrobe.org/h04c.files/history/aspergillus%20galactomannen.pdf)
- Fungal Infections - (http://www.life-worldwide.org/fungal-diseases/chronic-pulmonary-aspergillosis/)
- IDSA Practice Guidelines - (http://www.idsociety.org/uploadedfiles/idsa/guidelines-patient_care/pdf_library/aspergillosis.pdf)
What is Aspergillosis?
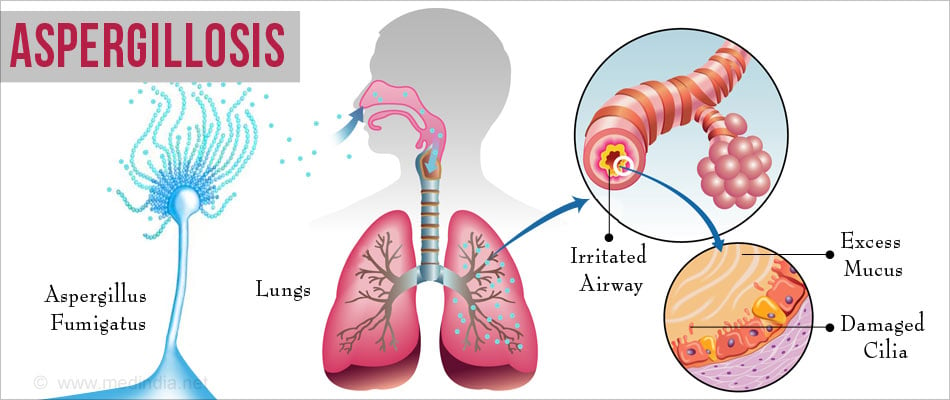
Aspergillosis is an infection or allergic reaction caused by the Aspergillus fungus. The Aspergillus fungus is widespread in nature and produces millions of tiny spores that are small enough to be inhaled.
The spores then settle and grow inside the airspaces of the lungs. Aspergillosis usually affects people with reduced immunity.
What are the Types of Aspergillosis?
The Aspergillus fungus is of several types like Aspergillus fumigatus, Aspergillus flavus, Aspergillus niger and Aspergillus terreus. Aspergillosis can affect the body in different ways and patients may exhibit different symptoms. Some of the manifestations of aspergillosis are the following:
Allergic Bronchopulmonary Aspergillosis (ABPA) is a potentially progressive disease resulting from an allergic response to the colonization of the respiratory system with Aspergillus fungus. ABPA occurs most commonly in patients with asthma or cystic fibrosis, affecting 2% and 1 to 15% patients, respectively. Some people who suffer from severe asthma but do not meet the criteria for ABPA are classified as severe asthma with fungal sensitization (SAFS).
Invasive aspergillosis is a disseminated infection affecting patients with weakened immune systems like those undergoing chemotherapy or suffering from conditions such as leukemia, other cancers, and AIDS. It starts in the lungs and sometimes the sinuses but may involve other organs and tissues through its spread via blood.
Chronic Pulmonary Aspergillosis (CPA) is an uncommon and slowly progressing destructive lung disease. It includes conditions like chronic cavitary pulmonary aspergillosis, chronic necrotizing pulmonary aspergillosis, and chronic fibrosing pulmonary aspergillosis. It usually affects one or both upper lobes damaging lung tissues and resulting in cavity formation.
Simple aspergilloma: Single (simple) pulmonary aspergilloma is the morphological appearance of a fungal ball, which occurs in a pre-existing cavity due to a disease like tuberculosis. There is no radiological progression over three months of observation.
Allergic Fungal Sinusitis (AFS) is the common type of fungal infection in the sinuses. The infecting fungi cause an allergic reaction which results in thick fungal debris and ultimately leads to blockage of the sinus.
Cutaneous aspergillosis is an infection by the fungus of the skin. The infection may result from an open wound, or may have spread from different parts of the body to the skin in disseminated aspergillosis.
What are the Causes of Aspergillosis?
Aspergillosis is the result of a combination of exposure to the Aspergillus fungus and a weak immune system. When common mold spores are inhaled, immune system cells surround and destroy them. But people with a weakened immune system from illness or immunosuppressant medications have fewer infection-fighting cells.
Exposure to Aspergillus is unavoidable and may occur from:
- Compost piles
- Stored grain
- Marijuana leaves
- Air conditioning, heating ducts
- Decaying vegetation
- Some food and spices
- Construction sites or building renovation sites
- Insulating materials (walls, ceilings, water cylinders)
Patients at increased risk for aspergillosis include those with:
- Tuberculosis
- COPD
- Sarcoidosis
- Lung cancer patients, including those undergoing treatment
- Patients with reduced immunity
- Cystic fibrosis
- Asthma

What are the Symptoms and Signs of Aspergillosis?
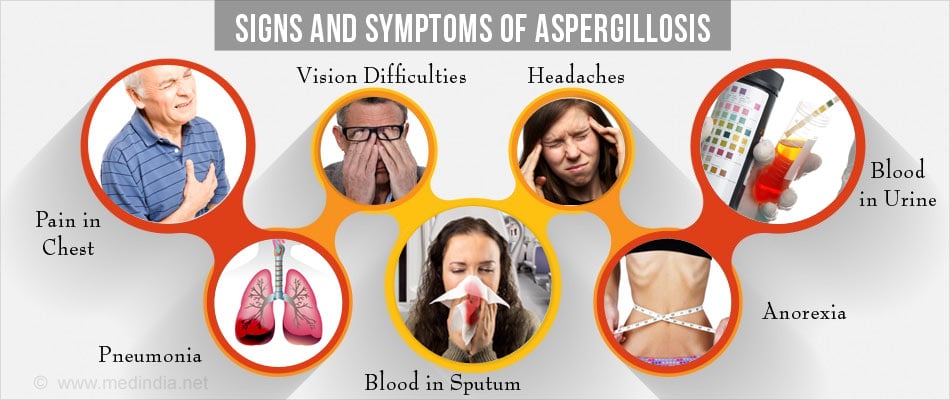
Different forms of Aspergillosis show different symptoms, but some common signs and symptoms may include:
- Pain in chest and bones
- Pneumonia
- Vision difficulties
- Blood in urine
- Less urine
- Headaches
- Chills
- Difficulty in breathing
- Cough with sputum production
- Blood in sputum
- Skin sores
- Anorexia and weight loss
How do you Diagnose Aspergillosis?
Diagnosing an infection caused by Aspergillus fungus can be difficult and depends on the type of aspergillus infection. Here are some tests that the doctor would suggest for a patient:
Imaging Test: A chest X-ray or computerized tomography (CT) scan - a type of X-ray that produces more-detailed images - may reveal if there are any cavities or fungal balls in the lungs.
Bronchoscopy and Biopsy: Bronchoscopy involves inserting a long, flexible tube with a camera at the end into the lung passages, via nose or mouth. During the procedure, a small piece of infected tissue (biopsy) may be removed to test for invasive aspergillosis.
Skin Prick Test: If ABPA or SAFS is suspected, skin prick test is usually done. The skin is pricked with a needle containing a small amount of aspergillus mold. If the person is allergic, the area of skin will develop a hard red bump.
Galactomannan Test: The diagnosis of invasive aspergillosis may be facilitated by a test for galactomannan antigen detection in the blood using an enzyme immunoassay. This test may be useful for patients with blood cancer, low white blood cell count.
Immunoglobulin E Test and Immunoglobulin G Test: Measurement of specific IgG and IgE antibodies for aspergillosis in the blood can help to diagnose aspergillosis.
Other tests that have been used in the diagnosis of aspergillosis include the (1→3)-β-D-glucan determination and polymerase chain reaction.
Respiratory Secretion (Sputum) Test: The sputum of the patient is stained with a particular dye and examined for the presence of Aspergillus filaments under a microscope. The sputum is also placed in a suitable culture medium that promotes the growth of the fungus.

How do you Treat Aspergillosis?
Antifungal compounds used for the treatment of invasive aspergillosis,
- Oral Itraconazole is an antifungal drug available as a capsule that helps to stabilize the clinical and radiological manifestations in patients with CPA.
- Voriconazole and D-AMB (deoxycholate amphotericin B) are drugs approved for primary treatment of invasive aspergillosis in the United States. Voriconazole is available as a tablet and as a solution for IV administration and is usually preferred. Liposomal formulations of amphotericin B are also available.
- Posaconazole is structurally similar to itraconazole and helps in prevention of invasive aspergillosis in certain neutropenic patients (patients with low white blood cell counts) or in patients with graft versus host disease.
- Studies suggest that there is patient-to-patient variability in the levels of drugs like itraconazole or voriconazole used for treatment or prevention of aspergillosis, which highlights the need for monitoring the drug levels in the blood via therapeutic drug monitoring. The necessity of therapeutic drug monitoring should be individualized depending on the clinical status of the patient and the overall treatment plans.
- Echinocandins: Caspofungin, Micafungin, and Anidulafungin. The echinocandins are a novel class of semisynthetic antifungals. Caspofungin is indicated in patients with probable or proven invasive aspergillosis. The recommended dosage of caspofungin in adults is a single 70-mg loading dose on day 1, followed by 50mg/day thereafter, administered by slow IV infusion of over a duration of 1 hour.

- Oral corticosteroids: Oral corticosteroids may be used in the treatment of allergic bronchopulmonary aspergillosis.
- Surgery: Surgery may be used in the treatment of aspergillosis that causes bleeding in the lungs. A procedure called embolization may as be used, in which the bleeding artery is blocked to stop the bleeding.
How do you Prevent Aspergillosis?
Aspergillus cannot be completely avoided in the environment and transmission by air is the commonest route, but the risk of infection can be reduced.
- Avoid places where Aspergillus spores are abundant - forests, gardens, compost heaps, grain stores, rotting vegetation, dead leaves, and building construction sites or renovation areas.
- The household environment and furniture surfaces should be kept clean, dust-free and dry in order to minimize the accumulation of fungus and molds.
- Avoid skin injuries. Any open wounds should be cleaned with antiseptic and covered with a clean dressing.
- In addition to this, good hygiene and a healthy lifestyle will help improve your body's immune defense against Aspergillus and other infections.
- Certain food items, such as spices and herbs, are usually found to contain Aspergillus spores, so they should be avoided.

Health Tips
- Allergic reaction can be harmful so medical advice should be done as soon as possible.
- Aspergillus fungi can also be found in air-conditioning systems and hospitals so people with reduced immunity should take extra care while going to such places.









