- American Academy of Ophthalmology Basic and Clinic Science Course (BCSC series) Section 11- Lens and cataract.
- Khairallah M, Kahloun R, Bourne R et al. N umber of People Blind or Visually Impaired by Cataract Worldwide and in World Regions, 1990 to 2010. Invest. Ophthalmol. Vis. Sci. 2015;56(11):6762-9.
- Allen D, Vasavada A. Cataract and surgery for cataract. BMJ : British Medical Journal. 2006;333(7559):128-32.
- Bourcier, Tristan, et al. "Robot-assisted simulated cataract surgery." Journal of Cataract & Refractive Surgery 43.4 (2017): 552-557.
- Avachat SS, Phalke V, Kambale S. Epidemiological correlates of cataract cases in tertiary health care center in rural area of Maharashtra. J Fam Med Primary Care 2014;3:45-7.
- Dhillon, Bal, and Gerassimos Lascaratos. "Age-related vision loss: cataract." Aging Health 5.6 (2009): 813-819.
- Saraiva, João, Kristin Neatrour, and George O. Waring IV. "Emerging technology in refractive cataract surgery." Journal of ophthalmology 2016 (2016).
- Hengerer, Fritz H., H. Burkhard Dick, and Ina Conrad-Hengerer. "Clinical evaluation of an ultraviolet light adjustable intraocular lens implanted after cataract removal: eighteen months follow-up." Ophthalmology 118.12 (2011): 2382-2388.
- Robinson, Michael L. "Lens, heal thyself: a significant advance in regenerative Ophthalmology." (2016).
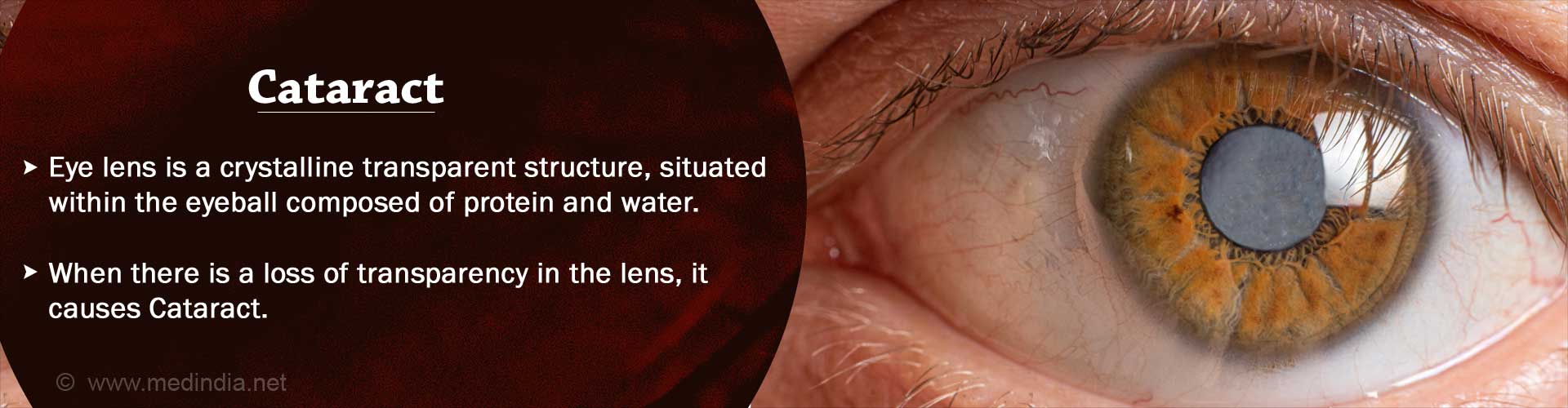
What is Cataract?
A cataract is any cloudiness in the crystalline lens of the eye or its overlying capsule.
When light enters the eye, it passes through the outer transparent dome called the cornea, then through the fluid behind the cornea in the anterior chamber called the aqueous humor, then the opening of the iris called the pupil, and then through a transparent lens and a thick gel-like fluid called the vitreous humor. These media help to focus the light onto the most sensitive part of the retina, which ensures clear vision.
The lens is located in a capsule just behind the iris and is suspended by fibers attached to the ciliary body. The ciliary muscles adjust the curvature of the lens to enable the eye to focus on objects at different distances. Clouding of the lens due to cataract prevents light from focusing on the retina and therefore affects vision.
Cataracts are examples of “curable blindness”. They cannot be reversed, meaning that the crystalline lens cannot become transparent again, but the visual impairment due to a cataract can be rectified by surgical removal of the lens and replacement with a synthetic intraocular lens.
Facts and Stats about Cataracts
About 20 million people in the world are blind due to cataract, which accounts for about 51 % of cases of blindness due to various causes. According to the latest statistics, blindness in one out of every three people and visual impairment in one in six people in the world is due to cataract. In India, cataract accounts for 62.6 % of cases of blindness.
What are the Causes of Cataract?
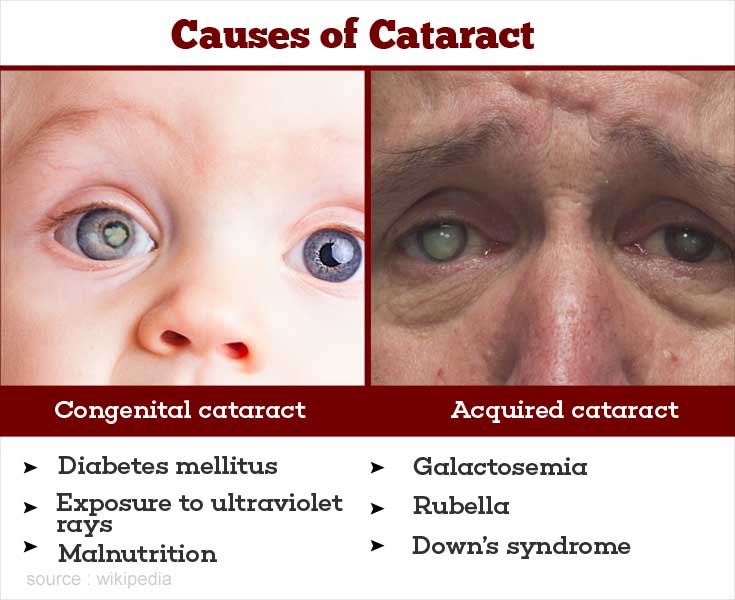
Age-related cataract, which appears at an older age, is the most common form of cataract. However, there are other causes as well. Broadly, cataract can be divided into congenital and acquired varieties.
Congenital cataract is cataract that is present from birth. Developmental cataract can develop shortly after birth. Some of the causes are – genetic, galactosemia, (presence of excessive galactose in the blood), Lowe syndrome (an inborn error of amino acid metabolism), congenital rubella (baby born to a mother who had German measles during pregnancy), congenital toxoplasmosis, cytomegalovirus or varicella (chicken pox) infection, Down’s syndrome, hypoparathyroidism, hyper- and hypoglycemia (increased or decreased sugar in the blood).
Acquired cataract is most commonly age related. Some of the other causes include – diabetes mellitus, myotonic dystrophy, malnutrition, atopic dermatitis, eye injuries, following eye inflammation, high myopia or short sightedness, and intake of drugs like corticosteroids. Some of the risk factors for age related cataract are –genetic factors, smoking, diabetes mellitus, exposure to ultraviolet B rays, deficiency of antioxidants like vitamins A,C and E, and severe dehydrating conditions at a young age.
What are the Types and Symptoms of Cataract?
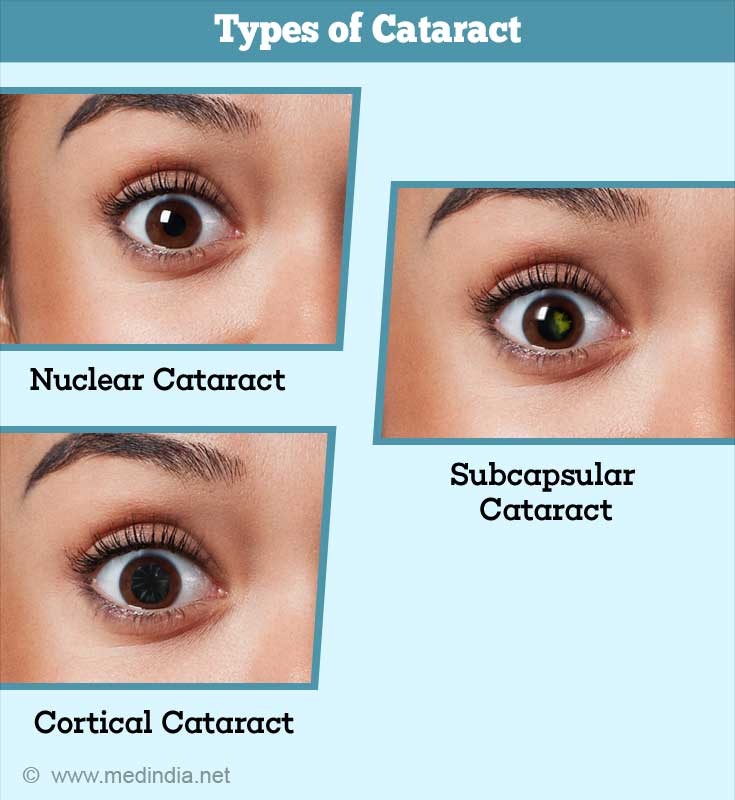
Age-related cataract is mainly of 3 types – cortical, nuclear and posterior subcapsular. Most patients have more than one of these types at the same time.
A posterior subcapsular cataract is cloudiness just in front of the posterior capsule of the lens. Because of its location (at the center of the visual axis), this type of cataract causes significant disturbances of vision even in its early stages, such as difficulty with near work, and impairment of vision in bright sunlight and during exposure to oncoming headlights during night driving.
Nuclear cataract
Here, there is a hardening of the center part (nucleus) of the lens. This results in short-sightedness referred as index myopia. Persons with an early nuclear cataract are often able to read without glasses (this temporary improvement in vision is referred to as “second sight”). Differential refractive indices in different portions of the lens can result in double vision or multiple images of the same object (often discernible as seeing multiple moons). In more advanced cases, difficult hue discrimination and impaired vision in the dark are experienced. Gradually, the vision is diminished enough to impair daily activities.
Cortical cataract
In a cortical cataract, the cloudiness or opacification is in the part of the lens lying superficial to the nucleus, and which is referred to as the cortex of the lens. Cortical cataracts occur due to coagulation of lens proteins. The symptoms depend on the location and density of the opacification. Patients frequently experience glare from oncoming headlights, double vision and a general impairment of distance vision that gets progressively worse with time.
How does a Cataract Progress?
A posterior subcapsular cataract gradually spreads from the center of the posterior part of the lens to extend more peripherally; it simultaneously also becomes denser, resulting in a significant impairment of distant vision. Nuclear cataracts become denser, more opaque and change in color from light yellow in the early stages to dark brown in advanced stages. However, though both these types of cataracts give rise to significant visual disability in the advanced stages, neither of them become mature. A cortical cataract, on the other hand, tends to progress in the degree of cloudiness, and eventually the entire lens becomes completely opaque. This is called a mature cataract. If surgical removal is not undertaken, further changes lead to hypermaturity.
What are the Complications associated with a Cataract?
Certain complications can occur in association with cataracts.
1. Phacomorphic glaucoma
Here, excess water accumulation in the lens either in the immature or mature phase results in the swelling of the lens to such an extent, that it pushes the iris forward, which then blocks the drainage of aqueous humor from the anterior chamber of the eye, resulting in a sudden rise in intraocular pressure. (The anterior chamber is the part between the cornea on the outside and the iris and the lens on the inside. It contains aqueous humor that is drained at the angle). The eye becomes red and painful, and needs to be treated by an eye doctor immediately.
2. Phacolytic glaucoma
Sometimes, in hypermature cataracts, the cortex of the lens becomes liquefied and leaks out through micro-perforations in the lens capsule. It is taken up by cells called macrophages, which then interfere with the drainage of aqueous humor from the eye. The sudden rise of intraocular pressure results in a red and painful eye and requires emergency treatment.
3. Lens induced uveitis
The leaked out lens material in hypermature cataracts can result in the formation of proteins called antibodies that result in a red, painful, inflamed eye. The eye doctor should be consulted immediately.
4. Hypermature cataracts can sometimes shrink, lose their support and then get either partially or completely displaced either forward or backward from their natural position. If they get caught in the pupil, there can be a dangerous rise of intraocular pressure, necessitating urgent treatment.
How do you Diagnose Cataract?
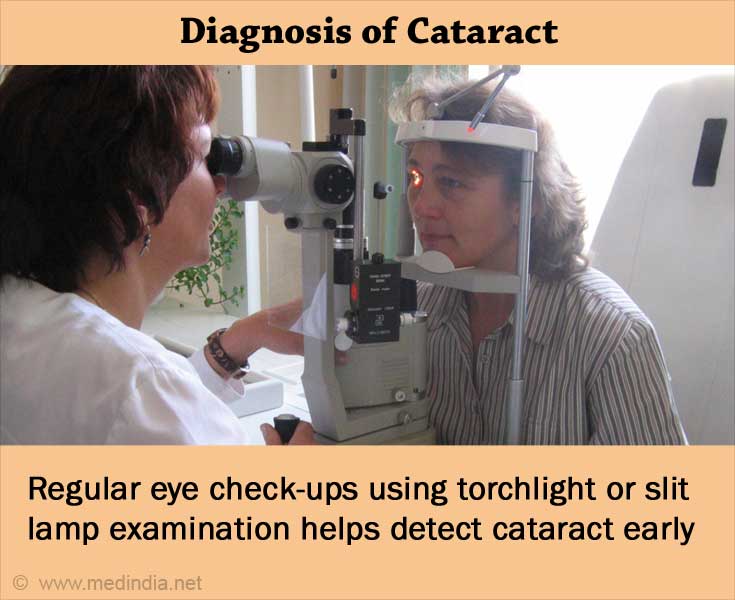
Cortical cataracts can usually be diagnosed with a simple torchlight examination. However, appropriate assessment of cortical and nuclear cataracts and the diagnosis of posterior subcapsular cataracts requires examination with the slit lamp. The examination is a painless procedure where the patient is asked to sit in front of the instrument and place the chin on a chin rest.
How do you Treat Cataract?
To date, there is no known medical treatment of cataract. There have been some clinical trials in the past few years which have studied the use of N-acetyl carnosine used as eye drops to halt the progression or reverse cataract. Some of these have shown positive results while others have not. Thus, there is no conclusive data at present to recommend this treatment for clinical use.
The definitive treatment of cataract today is the surgical removal of the crystalline lens with implantation of a synthetic IOL (intraocular lens – to replace the refractive function of the natural lens). Failure to place an intraocular lens results in a very high hypermetropia (long sightedness) which needs to be corrected either with spectacles or contact lenses for any useful vision to be present. Spectacles and contact lenses have many disadvantages; thus intraocular lenses are the gold standard for correction of vision after removal of cataracts.
Phacoemulsfication is the standard of care, and is the most commonly used surgical technique today to treat cataracts. An ultrasound driven probe is used to fragment the nucleus of the lens (which is hard) which is then sucked out of a very small (approximately 3mm) incision. A foldable intraocular lens is then introduced into the eye, usually by loading it into an injector. The lens unfolds in the eye. Since the incision is small and self sealing, sutures are not necessary. Thus, compared to older surgeries that required a larger incision and resulted in scarring, the chances of astigmatism (refractive error due to irregularities in the shape of the cornea) are largely reduced with the newer surgeries. . In MICS (micro-incision cataract surgery), the incision is less than 2.2 mm. Thus, the advantages of phacoemulsification are a sutureless surgery, very less chances of astigmatism, and a very quick post-operative recovery.
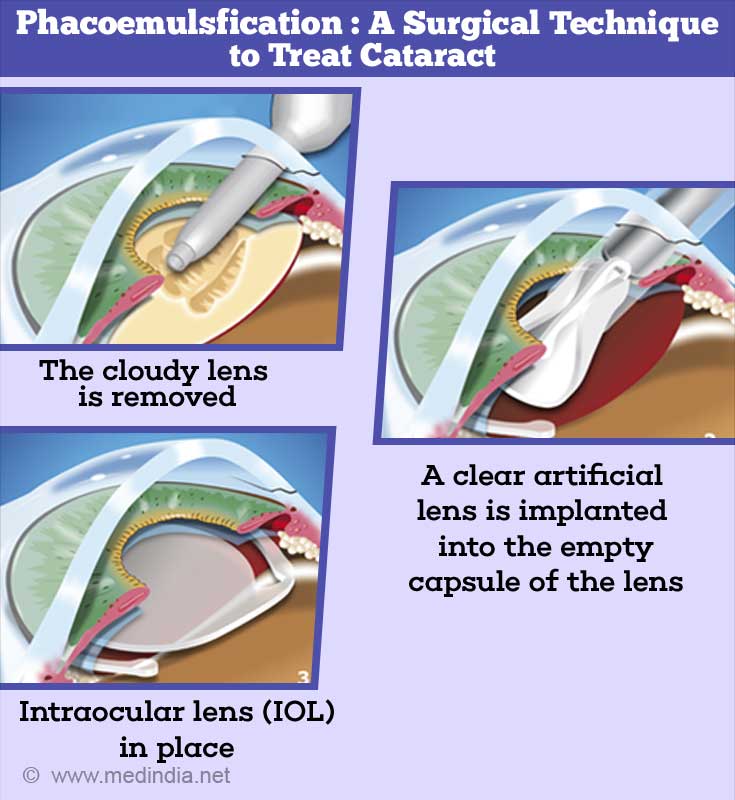
Overview of Phacoemulsification and IOL Implantation
Sometimes phacoemulsification may be difficult or not preferred because of the nature of the cataract. In such cases, a small incision cataract surgery (SICS) is carried out. Here, the incision is about 5.5 to 7 mm in length, but still does not require suturing if the incision is made as a self-sealing one. Also, a foldable lens is not required for an SICS.
The third type of surgery is what is described as an ECCE (extracapsular cataract surgery), wherein the surgical incision is much larger, and requires sutures to close it. This is very rarely performed these days as incidence of astigmatism is much higher in this type of surgery.
Cataract surgery is performed under local anesthesia, either by the instillation of local anesthetic eye drops, or by injection of the anesthetic into the tissue around the eyeballs. General anesthesia is only indicated in poorly cooperative adults and in children.
Femtosecond laser-assisted cataract surgery (FLACS) is gaining popularity in recent times. It uses intraoperative image guidance combined with short pulse delivery of a near infrared laser to achieve precise tissue dissection. In this, a femtosecond laser is used to replace manual performance of any or all of the following steps of cataract surgery – the corneal incision, capsulorrhexis (removal of the capsule of the lens), and lens fragmentation. This is what is commonly denoted by laser cataract surgery.
Recent Advances in Intraocular Lens Technology
Intraocular lenses are also available in newer designs. In contrast to the traditional monofocal lenses that correct vision only for distance (thus necessitating wearing of glasses for reading purposes), trifocals and multifocals allow intermediate vision and near correction in addition to that of distance. Another type of IOL is toric IOL, which can correct pre-existing astigmatism (these are akin to cylindrical spectacle lenses for astigmatism). Toric multifocals are also available. Various types of accommodating lenses attempt to respond to the accommodation effort of the patient in order to help in near vision. Various types of lenses that can correct residual post-operative refractive error with magnets, ultraviolet light (light adjustable lens or LAL) or laser are in clinical trials. Some of these are available in select countries, while others are in the trial stage.
Robot-assisted simulated cataract surgery is also being currently evaluated and shows some promising results. Lin and co-workers have attempted a slight modification of technique to aid in the regeneration of a clear lens in pediatric cataracts.
How do you Prevent Cataract?
There is no proven method today for preventing cataracts. Smoking and exposure to ultraviolet rays are avoidable risk factors in age related cataract. Cessation of smoking and the use of sunglasses may help in delaying the onset or progression of cataract. There is some suggestive evidence that intake of vitamins A,C, E, niacin, riboflavin, beta carotene and protein is protective. Lutein and zeaxanthin are carotenoids present in the human lens, and some studies have shown a decreased risk with foods rich in lutein such as spinach and broccoli.