Researchers at University of Manchester have found that less than seven percent of cervical cancer patients in the country receive the optimum treatment needed for eradicating the disease.
Dr Ian Hampson, from The University of Manchester's Institute of Cancer Sciences who oversaw the research, said the findings, published in PLOS One this week, add further weight to the call to spend more on cancer screening and prevention in Kenya.
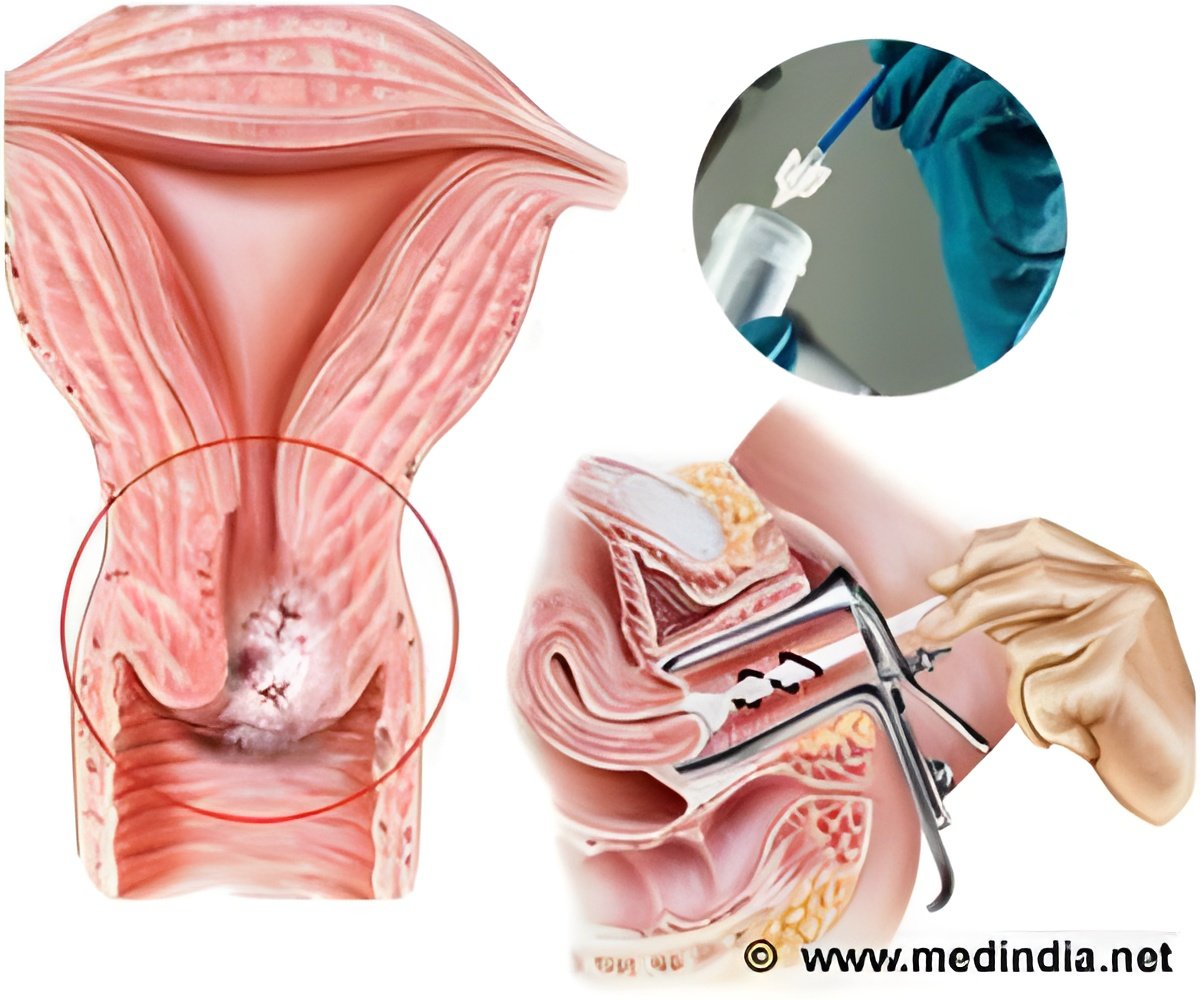
Cervical cancer is caused by infection with human papilloma virus (HPV) and is more than five times more prevalent in East Africa than the UK.
The Manchester researchers analysed treatment of 355 Kenyan women diagnosed with cervical cancer at the Departments of Gynaecology and Radiotherapy at Kenyatta National Hospital between 2008 and 2010. Of the 355 patients originally recorded, 146 (42%) disappeared during the two year period meaning they did not receive treatment. A further 64 (18%) of the remaining women died during the study period.
Dr Hampson said: "Our figures predict that less than 20% of those left will survive during the next two years. The late stage at which women get diagnosed, inaccurate assessments of the extent of the disease and long waiting times for treatment are all significant factors in this huge difference in survival rates between Kenya and the UK as well as poverty and lack of cancer awareness. Our study suggests simple, cost effective changes in hospital procedures to improve the situation."
The research team are now looking for more funders to help improve cancer treatment in Kenya, like The American company Hologic who have provided free HPV and cervical screening equipment plus running costs.
Advertisement
"The main issue is that, like many other low income nations, Kenya does not have a cervical screening program to detect the disease in its earliest stages or even the resources to treat this appropriately."
Advertisement
Dr Maranga, now consultant gynaecologist in Nairobi, has also established the Kenyan charity Cancer Research Trust- Kenya (CRT-K) with personal support from a UK philanthropist Ken Cholerton. CRT-K has contributed to the cost of cervical screening and also paid for the treatment costs of over 220 Kenyan women with advanced cervical cancer who could not afford this.
Dr Hampson, who is also part of Manchester Cancer Resdearch Centre (MCRC) a partnership between the University, The Christie NHS Foundation Trust and Cancer Research UK, added: "We have established a unique close working relationship between physicians/care-givers working in Nairobi and scientists and physicians in Manchester which gives us a golden opportunity to make a real difference in the lives of many Kenyan women afflicted with this disease. "We have made a fantastic start to tackling a very significant global health problem. We have assembled all the pieces of the engine – now all we need is the fuel to run it."
Source-Eurekalert