Dagfinn Aune, M.S., of Imperial College London, and colleagues conducted a review and meta-analysis to examine the association between maternal BMI (before or in early pregnancy) and risk of fetal death, stillbirth, and infant death. After a search of the medical literature, the researchers identified 38 studies that met criteria for inclusion in the meta-analysis, which included more than 10,147 fetal deaths, more than 16,274 stillbirths, more than 4,311 perinatal deaths, 11,294 neonatal deaths, and 4,983 infant deaths.
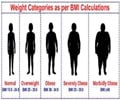
The researchers found that even modest increases in maternal BMI were associated with increased risk of fetal death, stillbirth, neonatal death, perinatal death, and infant death. The greatest risk was observed in the category of severely obese women; women with a BMI of 40 had an approximate 2- to 3-fold increase in risk of these outcomes vs. women with a BMI of 20.
The authors suggest that several biological mechanisms could explain the association found in this study, including that being overweight or obese has been associated with increased risk of preeclampsia, gestational diabetes, type 2 diabetes, gestational hypertension, and congenital anomalies, conditions that have been strongly associated with risk of fetal and infant death. "… further studies are needed to investigate the mechanisms involved."
"Weight management guidelines for women who plan pregnancies should take these findings into consideration to reduce the burden of fetal deaths, stillbirths, and infant deaths."
Source-Eurekalert