"The findings point to the need for improvements in prevention and treatment of transplant coronary artery disease that may help reduce restenosis for patients who require later cardiac procedures like stenting," said Dr. Michael Lee, an assistant professor of cardiology at the David Geffen School of Medicine at UCLA.
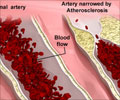
A stenting procedure begins with an angioplasty, in which a catheter is placed in an artery of the groin and a tiny wire is snaked up through the artery to the blocked area of the heart. The clogged artery is cleaned out, and then a stent — a tiny wire-mesh tube — is passed up through the artery and deployed to keep the artery open, allowing blood to flow freely through the heart again.
Currently, there are no guidelines or treatment recommendations for in-stent restenosis for transplant coronary artery disease, Lee said. He suggests that a scoring system to help pinpoint risks might help identify good candidates for stenting and other catheter-based procedures.
For the study, Lee and his team followed 105 heart transplant patients who underwent a stent procedure at UCLA Medical Center between 1995 and 2009. Patients received either a bare metal stent or, in the later years of the study, a newer medication-coated stent that can help impede restenosis development.
The team found that patients at a seven-year follow-up who had not developed in-stent restenosis were further from an end-point of death, heart attack or repeat transplantation (63.2 percent) than patients who had developed restenosis (27.9 percent). This was primarily due to a lower survival rate in patients who developed restenosis (38.5 percent) compared to patients who did not (84.2 percent).
Advertisement
Researchers note that the exact mechanism that heightens the risk of death and heart attack and increases the need for additional transplant in patients with transplant coronary artery disease who develop in-stent restenosis is not known.
Advertisement
"We may find that development of restenosis in heart transplant patients may be a marker of a more aggressive inflammatory response and part of transplant rejection," Lee said.
Further studies will help better understand the role of other factors in developing transplant coronary artery disease and in-stent restenosis.
Source-Eurekalert