The protein target identified in the RNAi screen described in the current study, Brd4—which contains a distinct domain or region known as a bromodomain—is a member of the BET family of proteins, which help regulate gene expression. By "reading" certain epigenetic marks or chemical tags attached to chromatin—the combined package of DNA and proteins around which it is coiled within the cell's nucleus—Brd4 helps control the pattern of which genes are switched on and how they work.
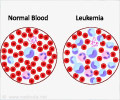
"Cancer is clearly a genetic disease, but we also appreciate that epigenetic changes in how genes are expressed contribute to the uncontrolled growth of cancer cells," says Vakoc. Cancer cells exploit this altered epigenetic landscape to drive their cell-growth programs.
Vakoc and other scientists have seized on the idea of interfering with this epigenetic dependency to turn the tables on cancer. "Epigenetic alterations acquired during cancer progression are potentially reversible and therefore susceptible to drug intervention," he explains. With this insight as the backbone of their strategy to find new therapies for cancer, "we began to systematically search for what the cancer needs to keep itself going, to find a way to shut down that cancer-fueling factor and develop a new therapy."
RNAi screening exposes chink in AML's armor
To do so, the team turned to RNAi screening in mouse models of AML, an approach developed and perfected previously in the laboratories of Scott Lowe and Greg Hannon at CSHL. In the RNAi screen, small hairpin-shaped pieces of RNA (shRNA) that can shut off specific genes—in this case, those that encode epigenetic proteins—are introduced into mice that harbor leukemia-causing mutations.
Advertisement
"Inducing an shRNA that shuts down a gene required for the survival of leukemic cells can lead to complete disease remission," explains Johannes Zuber, M.D., a former CSHL postdoctoral researcher in the Lowe laboratory who helped develop this approach and who has recently established his own group at The Research Institute of Molecular Pathology (IMP) in Vienna. "This ability to use shRNA to simulate the effect of an anti-cancer drug illustrates the power of this approach."
Advertisement
In a single experiment in which they screened more than 1000 shRNAs targeting 243 known epigenetic regulators of chromatin, the team of scientists focused in on one target–Brd4. Suppressing Brd4 with a shRNA led to a dramatic cell cycle arrest and death of leukemic cells, a marked delay in leukemia progression, and significantly extended the survival of leukemic animals.
Shutting down Brd4, the team confirmed, derailed a cellular process considered to be the hallmark of AML–the aberrant self-renewal of leukemic stem cells and their failure to complete their differentiation, or maturation, process. "We found that suppressing Brd4 in turn depletes the level and activity of a protein called Myc, which is thought to maintain leukemic stem cells," explains Junwei Shi, a graduate student in Vakoc's laboratory who worked with Zuber to spearhead these efforts.
A novel drug candidate for AML
These discoveries prompted a collaboration between the CSHL team and James Bradner, M.D., an oncologist and chemical biologist at the Dana-Farber Cancer Institute, who, serendipitously, had previously developed JQ1, a small molecular inhibitor of Brd4. Working together, the groups at CSHL and Harvard Medical School found that JQ1, which reproduced all the anti-leukemic effects seen in the Brd4 shRNA experiments, was an ideal drug candidate.
"Our extensive evaluation of JQ1 sensitivity in primary human leukemia samples and in established cell lines has revealed that this first-generation compound is broadly active against diverse AML subtypes," says Vakoc, who hopes that the second generation drug-like derivatives of the compound that are now being developed will have greater clinical utility in patients. "We're also excited to have found a pharmacological way to suppress Myc, which plays a role in many oncogenic pathways and is deregulated in most cancers," says Lowe.
"This study highlights the untapped potential of RNAi screening as a drug discovery platform, which Chris and other CSHL researchers are adapting to identify druggable targets for other types of cancers such as prostate and pancreatic cancers as well as melanoma," says CSHL President Bruce Stillman, Ph.D. "The success of this approach also points to the strength of the cancer research program at CSHL where our efforts in uncovering information about what drives individual cancers in patients is being rapidly translated into developing novel therapeutics that can immediately benefit patients in the clinic."
Source-Eurekalert