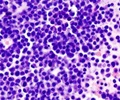
The drug thalidomide achieved infamy in the early 1960s as the cause of severe birth defects after being given to pregnant mothers for morning sickness. However, this drug, along with the highly related compounds lenalidomide and pomalidomide, also help to treat blood cancers, and are used worldwide as a cornerstone of therapy for the bone marrow cancer multiple myeloma. These drugs modulate the immune system and together are called immunomodulators or IMiDs.
The exact mechanisms and targets through which these therapies work to enhance immune response or kill cancer cells have been largely unknown. As a result, knowing which patients to treat and how to separate out the positive properties of these drugs from side effects has been impossible.
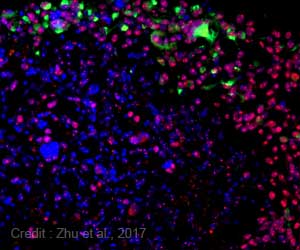
After recent research identified a protein known as cereblon as a primary mediator of the birth defects caused by thalidomide, researchers theorized that cereblon may also orchestrate the anti-tumor properties and be the primary therapeutic target for multiple myeloma.
In this study, researchers tested the theory and found a possible link between resistance to IMiDs and presence of cereblon. The researchers then found that lowering the level of cereblon allows the IMiDs to work properly.
"Interestingly, some resistant patients had normal cereblon levels, suggesting that while cereblon may be an absolute requirement for response, there are likely other mechanisms present that play a role in drug resistance," says Dr. Stewart. "These findings help us understand which patients may be more or less likely to respond to therapy and allow us to focus on other ways we can target cereblon as a possible biomarker to improve treatment and patient outcomes in multiple myeloma. This work also suggests that we can begin to dissect out the cause of birth defects from the anti-cancer properties and develop safer drugs in the future."
Advertisement
Source-Eurekalert