What is ECMO?
Extracorporeal membrane oxygenation (ECMO) is a technique used when both a person’s heart and lungs are in a life-threatening situation. It is an external aid through which the affected person’s blood is sent through to get purified. The device artificially removes the carbon dioxide from the blood and substitutes oxygen in place of it.
It is a supportive therapy and not a solution for an underlying disease process. It works best if the right patient, the right type of ECMO, and the right set up are involved.
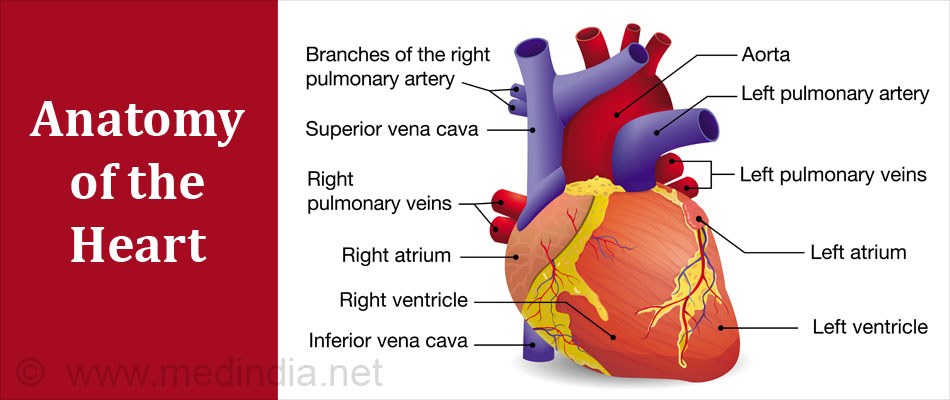
Brief history about the heart:
The heart is the organ responsible for pumping blood to the rest of the body.
The heart comprises of four chambers - 2 on the top called atria and 2 at the bottom called ventricles.
The four chambers can also be separated into the left and right compartments or sides of the heart, each side comprising of one atria and one ventricle.
Blood lacking in oxygen but abundant in carbon dioxide enters the heart through its right atrium and passes down to the right ventricle. The ventricle pumps the blood to the lungs through the pulmonary artery. In the lungs the blood gets purified and the carbon dioxide is exchanged for freshly inspired oxygen. From the lungs the blood returns to the left side of the heart through the left atrium. This oxygenated blood passes down to the left ventricle and then gets pumped out through the aorta to deliver blood to the entire body.
There are four valves in the heart. Two are present between the atrium and the ventricles to prevent backflow of the blood from the ventricles back to the atrium. The other two valves are situated at the base of the pulmonary artery and the aorta, again to prevent backflow.
ECMO is used as a support modality for primary or secondary diseases that cause respiratory or heart failures in newborns, children and adults.
ECMO does the job of making sure the blood gets oxygenated while helping the patient’s heart and lungs to rest and heal.
Indications for ECMO in babies and young children:
- Birth defects of the heart.
- Severe pneumonia.
- A life-threatening condition called sepsis where tissues or organs are injured due to the body’s response to infection.
- Air leaks that cause air to escape in the surrounding between the lungs and the chest cavity. This can cause breathing problems.
- Malformed diaphragm where the abdominal organs push into the chest cavity hindering lung formation. This is called congenital diaphragmatic hernia.
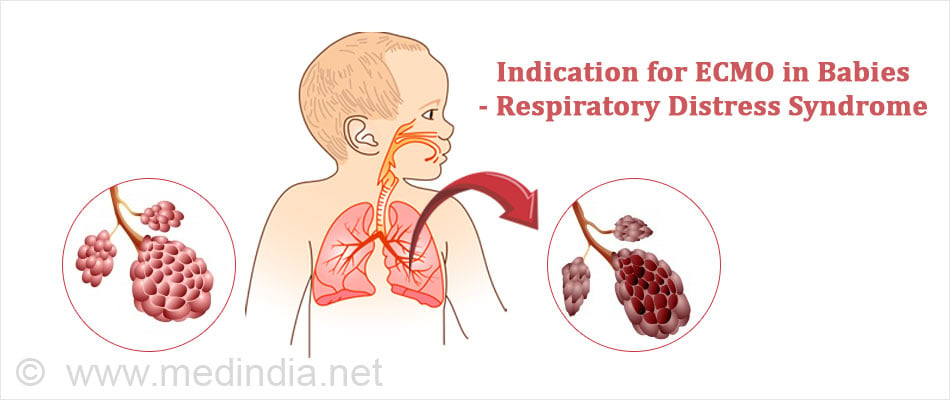
- A breathing disorder called respiratory distress syndrome that occurs in newborns who are born preterm or weigh very less.
- When the baby has aspirated its own stool or meconium present in the amniotic fluid because of a stressed labor or delivery (meconium aspiration).
- Pulmonary or lung-related hypertension that occurs because circulatory transition from fetal to extra-uterine life fails to occur. This is called persistent pulmonary hypertension.
- Congenital heart disease either prior or post of a cardiac surgery.
Indications of ECMO in adults:
The guidelines of Extracorporeal life support organization (ELSO) for the indications and practice of ECMO clearly state that this technique can be used only “if the patient has acute severe cardiac or pulmonary failure that is potentially reversible and that is unresponsive to conventional management”.
Such circumstances include:
- Cardiogenic shock caused by a heart attack or an ischemia; this causes decreased cardiac output.
- Cardiac arrest - ECMO for cardiac arrest is used in combination with cardiopulmonary resuscitation (CPR) and is known as extracorporeal CPR (E-CPR) to restore circulation.
![Indication for ECMO in Adults - Cardiac Arrest Indication for ECMO in Adults - Cardiac Arrest]()
- When patients cannot be weaned from cardiopulmonary bypass after a cardiac surgery,
- Cardiac support when complications like primary graft failure occurs post a heart or a heart-lung transplant
- As a bridge to
- Further treatments - this is done to give some time to doctors to check other organs like kidneys and the brain
- Transplant - this is done in a person with cardiac failure till the heart transplant or the left ventricular assist device (LVAD) transplant takes place. Can also be used in these patients till a decision is made on what the next step should be.
- To provide support during high-risk cardiac interventions
- Acute respiratory failure due to very low concentrations of oxygen or abnormally high carbon dioxide concentrations in the blood.
- As a bridge to transplant to tide over till a lung transplant operation takes place.
Hence a Candidate for ECMO is:
A person whose heart has failed due to a severe heart attack, pulmonary embolism (blockage of the pulmonary artery), bad valve disease or worsening heart failure.
A person whose lungs have failed due to pneumonia, lung cancer, pulmonary edema (fluid in the lungs), pulmonary embolism and chronic obstructive pulmonary disease (COPD).
The ECMO machine has a
- Blood pump that provides full blood flow to the patient
- An artificial membrane lung or an oxygenator
- Blood warmer and plastic tubing that connects each part.
In this procedure, the blue blood or oxygen deficient blood is taken out of the right side of the heart from the venous system and is pumped through the oxygenator. This device removes the impure carbon dioxide and pumps oxygen into the blood. The blood is warmed and pumped back into the body.
There are 2 types of ECMO:
Veno-arterial - VA ECMO is used during heart and lung failure. It is essentially a cardiopulmonary bypass and provides good oxygenation and ventilation. The blood is returned to the arterial system via the carotid artery in infants and children and via the femoral artery in adults. This method by-passes the heart and is hence used when the heart is failing.
Veno-venous - In VV ECMO blood is returned into the venous system. It is generally less risky and has fewer complications and preferred over VA ECMO. The oxygen that returns to a large vein has to travel through the heart to be pumped to the rest of the body via arteries. Therefore, it is imperative that the patient have a well-functioning heart.
Preparing for the ECMO Procedure:
- The patient is sedated and given pain medication.
- The patient receives an anticoagulant medicine called heparin during the procedure to keep the blood from clotting in the ECMO circuit.
- Special tubes called cannulae are inserted at specific locations into either an artery or a vein of the patient. This depends on the type of ECMO and the weight of the patient.
- X-rays are taken to ensure the tubes are in the right place.
- The patient is connected to a ventilator which keeps the patient from collapsing and the lungs to heal post ECMO.
While on the ECMO:
The patient has to be monitored by specially trained nurses, respiratory therapists, the surgeon and the surgical team to make sure they are stable and comfortable.
Vital signs, blood pressure and oxygen levels (especially to kidneys and the brain) are to be monitored.
Supplemental nutrition is provided intravenously or through a nasal-gastric tube.
Certain medications like antibiotics to prevent infections, diuretics to get rid of fluids, electrolytes to maintain salt and sugar balance and blood products if needed are given. Heparin and sedatives will be continued to be given.
Tests that should be continuously done are chest x-rays, echocardiograms and other blood tests.
An arterial blood test (ABG) is done twice a day to measure the oxygen level in blood.
Post ECMO:
- Surgical procedure to remove the tubes after performing tests to reassure that the heart and lungs are ready.
- Repairing of the vessels used in cannulation either inside or outside the operating room. Small stitches are used to close the spot where the tubes were placed.
- Ventilator might be left on if needed.
- Post ECMO, patients are kept in the ICU till they are stable and then transferred to their wards.
At the onset, patients who require ECMO support are high risk and potentially have a high predicted mortality. This coupled with putting them on an invasive therapy that involves cannulating the arteries and veins, providing systemic anticlotting and an extracorporeal bypass circuit adds up their risks.
The risks of the procedure have to be balanced against its potential benefits.
- Bleeding due to heparin that's given to prevent blood from clotting in the tubing.
- Infection and bleeding at the surgical sites.
- Clots or air bubbles in the tubings.
- Transfusion risks when given blood products.
- Risk of low blood flow to certain parts of the body in VA ECMO.
- Damage or death of any organ due to loss of blood or introduction of air into the system - this can occur due to mechanical failure.
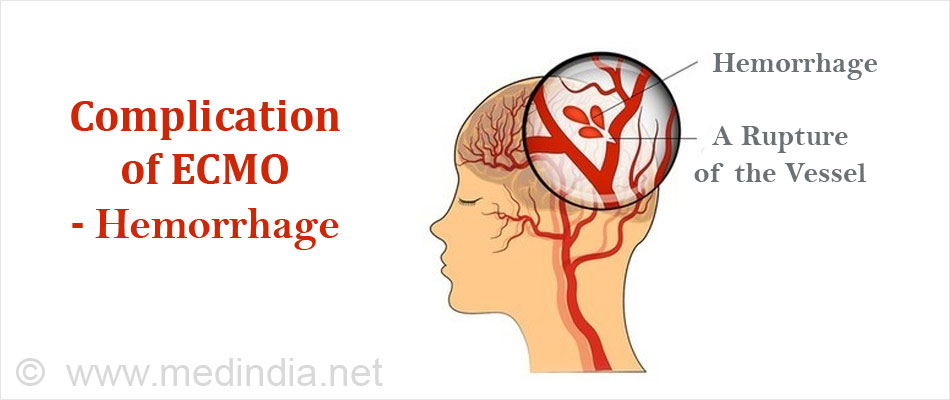
- Neurological complications like hemorrhage or stroke.