Serological Examination
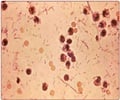
Antibodies to Malaria are detected by Enzymatic Immunoassays or Immuno fluorescence techniques.
- Antibodies of the asexual blood stages appear days to week after the infection and may persist for month.
- Indirect Fluorescent Antibody (IFA) test is used to detect antibodies against plasmodium. Due to presence of antibodies for long period in the blood, it is not of practical routine diagnostic test for malaria, but it may be useful for:
- Screening of blood donors prior to blood transfusion to avoid transmission of infection.
- To monitor the prognosis of the disease and evaluation of treatment method.
Dip - stick Technique:
Dip stick analysis of
This method is a rapid and accurate method for detection of P. falciparum infection.
It requires almost no training for performing the test in laboratories.
Disadvantage of the test is the presence of circulatory antigen for many days even after elimination of viable parasite. This test is still being established.
Molecular Diagnosis:
This technique considered far more reliable and precise than the microscopic technique, is required to be performed in well- equipped laboratories. Undoubtedly, an expensive diagnostic tool, this test involves the detection of specific parasite Nucleic acids done by Polymerase Chain Reaction (PCR).
Drug Resistance Tests:
In vitro drug resistance tests are performed to gauge the efficacy of the drug against the malarial parasite.
In vitro tests: These tests are equipped to assess the least concentration of the drug required to be successful in quelling the growth of the parasite in a culture medium.
In vitro Molecular detection: Encompass molecular tests conducted to assess the extent of resistance to drugs.
Diagnosis of Malaria poses a huge challenge in the following circumstances:
- In non endemic areas, diagnosis of malaria poses a huge challenge as doctors may not recognize the need for additional investigatory evaluations, due to the non familiarity of the disease and its symptoms.
- Laboratories in non-endemic areas are not familiar with the detection of malarial parasites in the blood smears under the microscope and may miss the diagnosis.
- Some carriers do not show any symptoms of Malaria infection as they have partial immunity against malarial parasites, and do not manifest the infection.
- In endemic countries, lack of resources, doctors, equipments causes problems in early detection of malarial parasites.