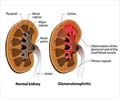
Q: What type of vasculitis affects the kidney?
A: The kidney in particular is affected by small vessel vasculitis (SVV), which may involve the tiny blood vessels in the filtering units of the kidney. Inflammation of these filters is called glomerulonephritis. It is a common cause of a severe but treatable kidney disease called crescentic nephritis, because of the appearance under the microscope. This is also called rapidly progressive glomerulonephritis (RPGN) because of the speed with which it can cause kidney failure.
Q: Do I need dialysis?
A: In severe Small Vessel Vasculitis (SVV), it is common for dialysis to be required soon after the diagnosis is made. However, treatment can often heal severe kidney disease, so that, dialysis is no longer required.
Q: What are ANCA?
A: Antibodies are molecules that are found in the blood stream in order to fight infection, by targeting foreign molecules and are often found in the blood of patients with small vessel vasculitis (SVV). ANCA (Anti-Neutrophil Cytoplasmic antibodies) stick to molecules found in white blood cells rather than to foreign material. The presence of these antibodies is very helpful in the diagnosis.
Q: Can Vasculitis be completely cured?
A: With the improvement in better medical treatment, it is now possible for people to live with Vasculitis. As there is no complete cure at present, it is important to understand that it is a lifelong condition. On medication, the disease condition may become quiet for sometime which is called relapse, after which a period of remission occurs where the disease conditions reappear. The rate of relapse and remission varies between different types of vasculitis, and your doctor takes this into consideration when prescribing a treatment regime (i.e., what medicines are needed when and for how long).
Q: What is Giant Cell Arteritis (GCA)?
A: This condition usually occurs in people older than 50, it results in inflammation of the arteries in your neck, upper body, arms, and — most often — head, especially the temples. GCA is the most common type of vasculitis in the United States and can cause headaches, scalp tenderness, jaw pain, blurred or double vision, and even blindness. GCA is often associated with polymyalgia rheumatica, stiffness and aching in the neck, shoulder and hip girdle regions.