- Khurram Bari and Guadalupe Garcia-Tsao. Treatment of portal hypertension. World J Gastroenterol. 2012 Mar 21; 18(11): 1166–1175.
- Huang HC, Lee FY and TI Huo. Major adverse events, pretransplant assessment and outcome prediction. Journal of Gastroenterology and Hepatology 24 (2009): 1716–1724.
What is Portal Hypertension?
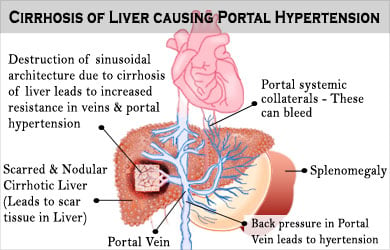
The portal venous system refers to the veins that drain blood from the intestines, stomach, pancreas, esophagus and spleen into the liver prior to entering the main or systemic circulation. All ingested nutrients, drugs, toxins and infectious agents are absorbed by the intestines and sent to the liver via the portal vein for appropriate processing or detoxification and the filtered blood leaves the liver via the hepatic veins draining into the vena cava. The portal venous system is normally a low pressure circuit, but if there is constriction or obstruction of the veins, then the pressure rises causing portal hypertention.
A blockage of portal venous flow leading to portal hypertension can occur before entering the liver, inside the liver or after leaving the liver, but the most common cause of portal hypertension is liver cirrhosis. When the portal pressure rises significantly, the body attempts to correct the situation by forming collateral routes between the portal and systemic circulations. A host of complications ensue, the three most common being encephalopathy (confusion), ascites (abdominal fluid retention) and gastroesophageal varices (thin walled blood vessels prone to rupture and fatal bleeding). Portal hypertension is a highly morbid and often fatal condition, but many successful treatments exist to manage the associated symptoms or to completely cure the problem.
What are the Causes of Portal Hypertension?
Causes of portal hypertension can be classified as pre-hepatic, intra-hepatic and post-hepatic. Hepatic is a medical term for liver. Hence prehepatic is any casue that blocks the portal vein before it enters the liver and similarly post-hepatic means blockage after the vein leave the liver.
Pre-hepatic causes include:
- Portal vein thrombosis
- or Congenital atresia (failure of the main portal vein to form properly during fetal development)
While congenital atresia is quite rare, portal vein thrombosis is not uncommon, occurring in up to 20% of patients with liver cirrhosis.
Intrahepatic causes include:
- Liver cirrhosis
- Hepatic fibrosis (due to Wilson’s Disease, hemochromatosis or congenital fibrosis)
Non-cirrhotic causes such as:
- Schistosomiasis
- Massive fatty change
- Idiopathic non-cirrhotic intrahepatic portal hypertension (NCIPH)
- Diffuse granulomatous diseases (tuberculosis or sarcoidosis).
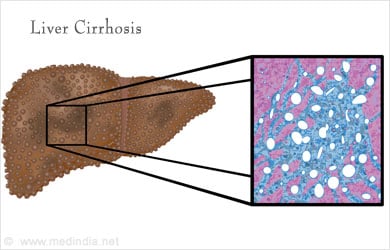
There are many causes of liver cirrhosis, including viral hepatitis (Hepatitis B or Hepatitis C), alcoholic liver disease, fatty liver disease, autoimmune diseases (Primary Biliary Cirrhosis or Sclerosing Cholangitis) and genetic defects (Alpha-1 Antitrypsin deficiency or hemochromatosis). When the liver is subjected to constant injury and inflammation, scar tissue forms starting with fibrosis then ultimately leading to end-stage scarring or cirrhosis. The hardened, scarred liver impedes the incoming portal venous flow and the portal pressure rises.
Post-hepatic causes - can occur at any level between the liver and right heart, including:
- Hepatic vein thrombosis,
- Inferior vena cava thrombosis,
- Inferior vena cava congenital malformation
- Constrictive pericarditis.
These causes are rare but do not necessarily involve chronic liver injury, so the prognosis of these entities is better compared to intrahepatic causes (if the diagnosis is made promptly and appropriate treatment is rendered).
What are the Symptoms of Portal Hypertension?
Signs and symptoms of portal hypertension include:
- Hepatic Encephalopathy
- Ascites

- Portal variceal bleeding
- Hepatorenal syndrome
- Hepatopulmonary syndrome
- Portopulmonary hypertension
- Splenomegaly
- Increased spontaneous bacterial peritonitis risk
What is Encephalopathy?
Encephalopathy refers to neuropsychiatric changes ranging from mild confusion to full coma and is caused by portal blood flow failing to reach the liver for adequate detoxification. Bacterial toxins in the gut, including ammonia and other substances such as gamma-aminobutyric acid (GABA) are normally neutralized in the liver.
In portal hypertension, the excessive portal flow bypasses the liver and enters the systemic circulation via shunts between the portal and systemic venous systems. These neurotoxins then accumulate in the brain and cause encephalopathy.
What is Ascites?
Ascites or accumulation of intraabdominal fluid, is caused by increased hydrostatic pressure from the portal system (leading to fluid “weeping” from the surface of the liver) and decreased oncotic pressure from low albumin levels in the diseased liver (albumin is the major protein produced by the liver). Extreme fluid accumulation causes discomfort, difficulty breathing and decreased appetite. The heart and kidneys can ultimately become damaged if the process is unchecked.
Understanding Portal Variceal Bleeding
Portal variceal bleeding is caused by collateral circulation engorgement of veins, particularly in the esophagus and stomach, leading to thin walled “varices” that are prone to rupture. Esophageal varices are seen in up to 60% of patients with advanced (or “decompensated”) cirrhosis and variceal bleeding is the most feared complication of portal hypertension because blood loss can be rapid and fatal with an overall mortality rate of 20% per bleeding episode.
Hepatorenal syndrome (HRS) & Hepatopulmonary syndrome (HPS) as a complication of Portal Hypertension
Hepatorenal syndrome (HRS) occurs when vasodilation of the “splanchnic” (gastrointestinal) circulation decreases blood flow to the kidneys, ultimately leading to renal failure. Early onset HRS is often reversed with a liver transplant, but long term HRS can completely shut down the kidneys, necessitating hemodialysis.
Hepatopulmonary syndrome (HPS) is a rare complication of portal hypertension and is caused by shunting of intrapulmonary arterial to venous blood flow, resulting in hypoxemia (low blood oxygen levels) and difficulty breathing.
Portal pulmonary hypertension results from the “remodeling” of the pulmonary vasculature, leading to excessively high blood flow in the pulmonary circulation. This complication has a high mortality rate but it is fortunately quite rare.
What is Splenomegaly?
Splenomegaly, or an enlarged spleen, occurs in portal hypertension because the portal flow backs up and impedes proper drainage of the splenic vein. Splenomegaly is associated with thrombocytopenia (low platelet count) and sometimes pancytopenia (low platelet, red blood cell and white blood cell counts). Thrombocytopenia increases the risk of bleeding because platelets are the cells responsible for forming blood clots. Pancytopenia can be associated with an increased infection risk.
Spontaneous bacterial peritonitis (SBP) is an infection of the abdominal cavity and fluid surrounding the abdominal organs. Patients with chronic ascites are at high risk for SBP.
How to Diagnose Portal Hypertension?
Physical exam and laboratory evaluation usually will give the first clues that portal hypertension is present in the case of cirrhotics.
On Physical Examination - A small, shrunken liver, enlarged spleen and ascites are evident on abdominal palpation. Significant splenomegaly will always result in thrombocytopenia. A history of underlying liver disease, such as chronic hepatits viral infection, heightens suspicion of the diagnosis. In cases of noncirrhotic portal hypertension, the liver often appears normal but ascites and splenomegaly are still present.
Lab Tests – A Blood count, electrolytes, Urea, Creatinine and Live Function Tests are required along with a routine urine test.

Imaging Tests- Imaging studies, either ultrasound, CT or MRI, will reveal a shrunken liver with irregular edges, splenomegaly and ascites, but the formal diagnosis of portal hypertension is made invasively.
A pressure transducer catheter can be inserted into the portal vein to directly measure the pressure, but this is dangerous because of the bleeding risk. Most of the time, the portal pressure is measured indirectly by placing a balloon catherter in the hepatic vein (accessed via the jugular vein in the neck) and measuring the hepatic vein wedge pressure gradient (HVPG). A value above 5 mmHg is diagnostic of portal hypertension and symptomatic portal hypertension occurs when the HVPG rises above 10 mmHg.
What are the Treatment for Portal Hypertension?
Effective symptomatic treatment exists for the management of portal hypertension complications.
Encephalopathy can be controlled with lactulose, a bowel evacuating agent that decontaminates the gut, and rifaxamin, a nonadsorbable antibiotic that decreases the amount of gut bacteria.
Ascites can usually be successfully managed with a combination of diuretics (furosemide plus aldactone is the most common combination). Sometimes it is necessary to drain the ascites using a needle through the skin into the abdominal cavity (“paracentesis” or “tap”), but excessive paracenteses increases the risk of bleeding and infection.
Esophageal varices are managed with frequent endoscopies by a gastroenterologist or hepatologist in which large varices can be ablated using rubber bands or injection of sclerosing agents such as alcohol or glue. Patients are also prescribed beta blockers to reduce the pressure in the varices.
If an infection is causing portal system obstruction such as tuberculosis or schistosomiasis, appropriate medications are prescribed to eradicate the infection.
If a blod clot is present in the portal vein or hepatic veins, then anticoagulants such as Coumadin or heparin may be prescribed, but chronic clots are usually not responsive to these medicines. “Clot busting” drugs such as tissue plasminogen activator (tPA) can also be directly infused into the thrombosed vessels by the Interventional Radiologist, but again, such interventions are most successful with fresh clots. Mechanical removal of clots, with or without angioplasty and stenting can also be attempted under appropriate circumstances.
The transjugular intrahepatic portosystemic shunt (TIPS) procedure has emerged over the past decade as the first line treatment for immediate resolution of portal hypertension. This minimally invasive procedure is performed by the Interventional Radiologists either in the radiology suite or operating theater, depending on whether local anesthetic and sedation or general anesthesia are required (usually the former). A catheter is placed into the jugular vein and directed down into the liver via the hepatic veins. Then a passage is created between the hepatic vein and portal veins within the liver. An expandable wire mesh stent is positioned to allow portal blood to flow directly into the hepatic vein. This procedure immediately decompresses the portal venous system. A TIPS can be life saving in the face of a massive esophageal variceal bleed. Associated ascites and renal insufficiency are almost always reversed, but the procedure can worsen encephalopathy and the shunt needs to be monitored regularly for patency. Further interventions may be needed to keep the TIPS open.
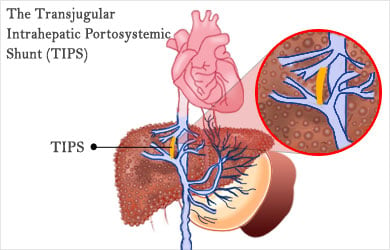
Surgical shunts for portal hypertension involve making a connection between the portal and systemic venous systems, either directly or using synthetic graft material. Surgical shunts have become much less common in the era of TIPS.
Liver transplant is the ultimate cure for portal hypertension caused by cirrhosis or venous thrombosis. Not only is the diseased liver removed, but the portal pressure in the newly transplanted liver is normalized. A successful liver transplant results in normal hepatic function, resolution of encephalopathy and ascites, collapsing of gastrointestial varices and shunts, and normalization of the platelet count.
Recovery
A TIPS procedure often requires an overnight stay in the hospital for observation, but sometimes can be done as an outpatient. Recovery from a surgical shunt procedure or liver transplant can involve a hospital stay anywhere from 7 to 14 days (longer if there are any complications) and complete recovery from a liver transplant takes about 3 months.









