- About PELVIC FLOOR DYSFUNCTION - (http://www.ichelp.org/about-ic/associated-conditions/pelvic-floor-dysfunction/)
- Pelvic Floor Dysfunction Expanded Version - (https://www.fascrs.org/patients/disease-condition/pelvic-floor-dysfunction-expanded-version)
- More on Pelvic floor dysfunction - (https://en.wikipedia.org/wiki/pelvic_floor_dysfunction)
- Pelvic Floor Disorders - (http://www.uchospitals.edu/specialties/pelvic/faq/pelvic-floor-disorders.html)
- Pelvic Floor Dysfunction - (https://my.clevelandclinic.org/health/diseases_conditions/hic_pelvic_floor_dysfunction)
- Pelvic Muscle Exercises - (http://www.voicesforpfd.org/p/cm/ld/fid=25)
What is Pelvic Floor Disorder?
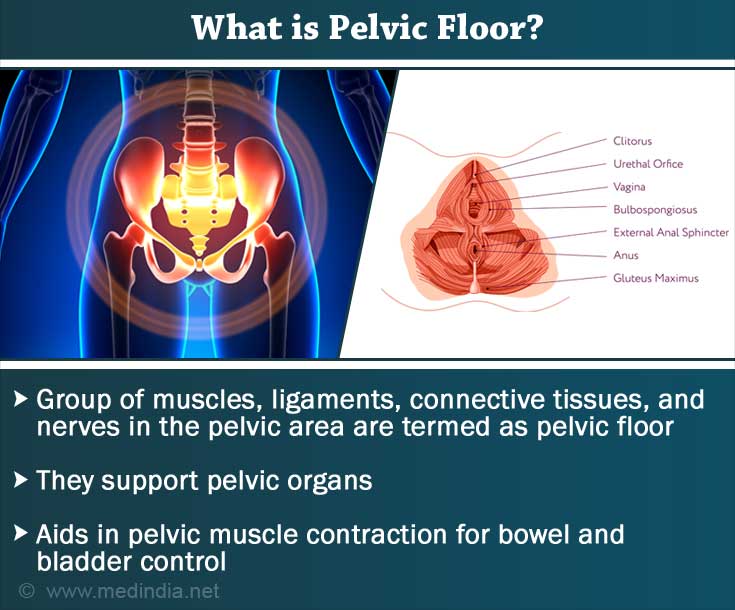
Pelvic floor disorder encompasses a group of disorders that cause abnormalities of bowel storage and emptying of bowel as well as pain in the pelvic region. The muscles of the pelvic floor become weak or tight. Impairment of the sacroiliac joint, lower back, coccyx or hip joints may also cause pelvic floor disorders. The clinical conditions associated with pelvic floor disorders include urinary incontinence, fecal incontinence, pelvic organ prolapse, sexual dysfunction, chronic pain in the muscles of the pelvic floor.
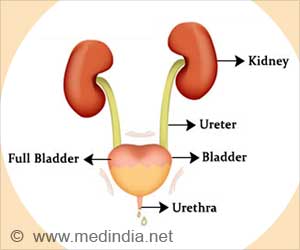
Pelvic floor is the collective term for the group of muscles, ligaments, connective tissues and nerves in the pelvic area. The muscles and tissues support the pelvic organs like bladder, uterus, prostate and rectum. These muscles contract to control bowel and bladder movements.
Pelvic organ prolapse is a condition in which organs such as uterus, bladder or bowel may “drop” onto the vagina and cause a bulge through the vaginal canal. The organ may descend below the pubococcygeal line causing the bulge. Pelvic floor has two hiatuses or gaps – urogenital hiatus through which the urethra and vagina pass through, and rectal hiatus through which the anal canal passes.
Kegel exercises for women are known to be effective for pelvic floor disorders.
What are the Causes of Pelvic Floor Disorders?
Postpartum pelvic floor dysfunction is a common occurrence in women. Studies have revealed that pregnancy is the cause of the incontinence for many women and is not associated with vaginal or cesarean delivery.
Other risk factors for developing pelvic floor disorders include obesity and menopause. Some may have congenitally weak connective tissue and fascia and stress, thus making them prone to stress urinary incontinence and pelvic organ prolapse. Inherited deficiency of the collagen type is also a factor that causes the pelvic floor muscles to be weak, leading to pelvic floor disorder.
Some of the specific conditions that may result in pelvic floor disorders include:
- Rectocele: Prolapse (slipping forward) of the wall between the rectum and vagina.
- Paradoxical Puborectalis contraction: Wrongly angled puborectalis muscle (muscle connecting the rectum to pubic region) resulting in a lack of straightening of anorectal angle (angle of anus and rectum) and poor opening of the anal canal.
- Levator syndrome: Pain in rectal area caused by spasm of the Levator ani muscle. Coccygodynia, pain in the tailbone; and Proctalgia fugax, fleeting pain in the rectum are the variants of Levator syndrome.
- Pudendal neuralgia: Pudendal nerve runs through pelvic region, including genitals, urethra, anus and perineum. Any problem in the nerve can cause severe, sharp pain along the course of the pudendal nerve, especially while sitting.
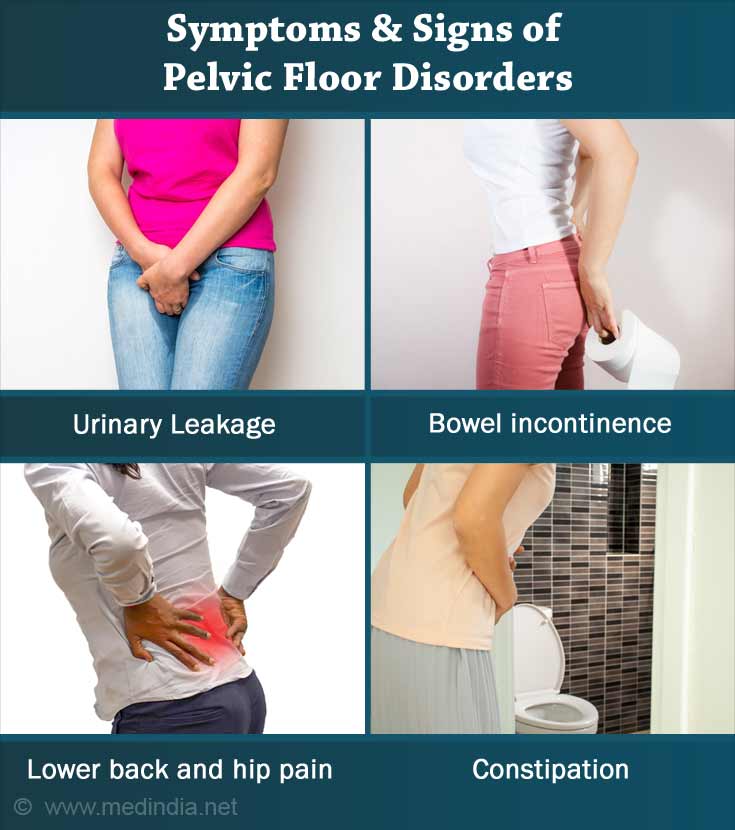
What are the Symptoms and Signs of Pelvic Floor Disorders?
Symptoms of pelvic floor disorder include:
- Lower back and hip pain
- Urge to have several bowel movements in a short period of time.
- Abnormalities in bowel storage
- Constipation or straining pain during bowel movement and bowel emptying
- Frequent urge to urinate without a continuous flow of the urine.
- Pain during urination.
- Constant pain in lower back, pelvic region, rectum or genitals.
- Painful sexual intercourse (in women), during sexual stimulation and orgasm.
- Urinary incontinence
- Fecal incontinence
- Pain or pressure in vagina or rectum
- Feeling of bulge in the vagina or rectum
- Pelvic muscle spasms
How to Diagnose Pelvic Floor Disorders?
Diagnosis of pelvic floor disorders includes patient history, physical examination and diagnostic tests.
Patient history:
Information on the following help in the diagnosis of pelvic floor disorders:
- History of urinary tract infections
- Pregnancy history
- Type of childbirth (prolonged, forceps, cesarean section, perineum tear or episiotomy)
- Irritable bowel syndrome and interstitial cystitis (to be ruled out)
- Pain during intercourse
- Abnormal bladder or bowel movements
Physical examination:
- Palpation of any bulge in the vaginal canal
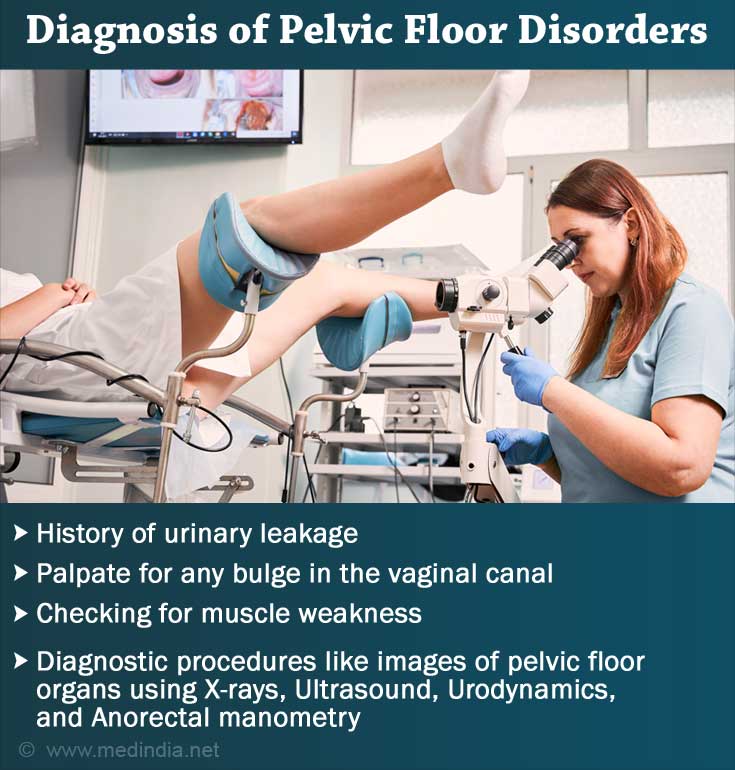
- Checking for muscle spasms, muscle knots or muscle weakness
- Checking muscle control with surface electrodes on the perineum or sacrum
Diagnostic procedures:
- Endorectal ultrasound: Ultrasound testing by inserting probe into the anus and rectum.
- Anorectal manometry testing: Inserting a flexible catheter into the rectum to evaluate the voluntary contraction of anal sphincter muscle and the reflexes of the anus and the rectum.
- Pudendal nerve motor latency testing: Pudendal nerve is stimulated at the anus, by inserting an electrode placed on the tip of the examiner’s finger. It evaluates the function of the nerves to the pelvic floor and anal sphincters.
- Electromyography: Evaluating the activity of the nerves and muscles of the anal sphincter and pelvic floor.
- Video defecography: An enema of thickened liquid contrast is given to the patient and a special x-ray takes video pictures of the bowel movements while the patient sits on a commode. It records the movement of the muscles of the pelvic floor.
- Colonic transit study: Contrast medium is swallowed and is released stage by stage at defined periods of time (for example, days 1, 3 and 5). The movement of the contrast through the colon is tracked. It evaluates the colon motility and the site of obstruction in constipation.
- Balloon expulsion test: A small rubber balloon is placed into the rectum and filled with water. The patient is asked to sit on a commode and expel the balloon. Failure to do so can indicate obstruction during defecation.
How do you Treat Pelvic Floor Disorders?
Treatment of pelvic floor disorders involves a combination of self-care, medications, physical therapy and muscle strengthening exercises.
Self-care: Counseling is done about self-care and advice is given not to strain or push while urinating and defecating. Keeping the pelvic floor muscles relaxed is important. The patient is also advised to maintain a good posture to avoid pressure on the bladder and pelvic organs.
Medications: Low doses of muscle relaxants like diazepam are prescribed for persons who find it difficult to relax.
Biofeedback: The patient is asked to attempt to relax and contract the pelvic floor muscles. The movements of the pelvic floor muscles are monitored by special sensors and video monitor. The patient is encouraged to perform voluntary contractions of the muscles and the therapist provides feedback to improve muscle coordination.
Physical Therapy and Exercises: Exercises for improving muscle strength and coordination in patients with pelvic floor disorders are done with the help of a physical therapist who is specially trained in pelvic floor rehabilitation. The therapy may involve the following techniques.
- Manual maneuvering of the muscles related to the pelvic floor dysfunction for improving strength and preventing wasting of muscles.
- Using various devices that help in relaxing pelvic floor. Some of them include cold laser therapy, ultrasound and interferential therapy for pain relief. Electrical stimulation to desensitize the muscles is also used.
- Training in exercises to be done at home on a regular basis. They include techniques to relax the pelvic floor, maintaining a good posture and learning to sense the pelvic floor muscles and relax them.
Some of the physical exercises that can be done for pelvic floor disorders include:
- Kegel exercises for women
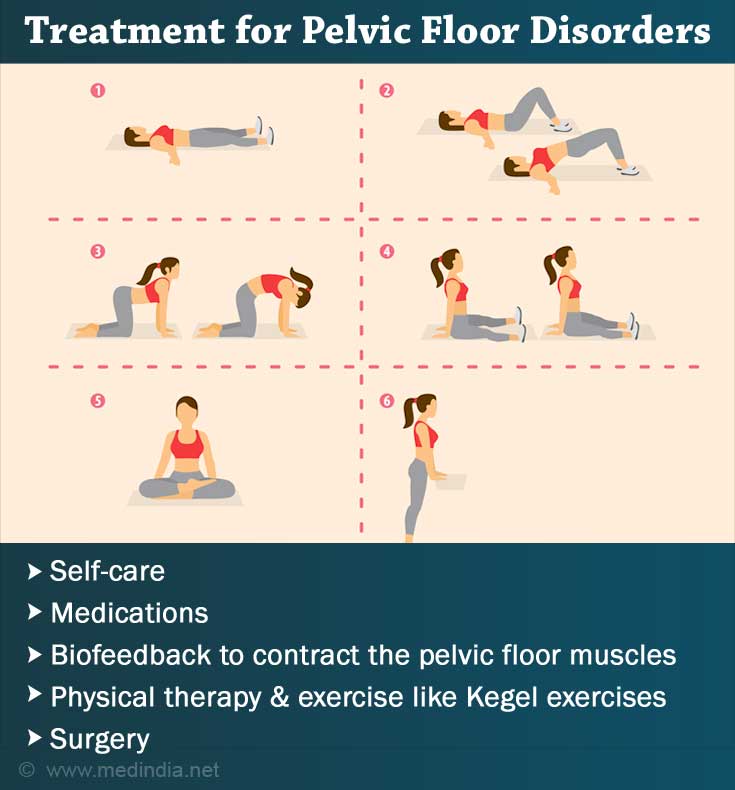
- Internal massage done by the physical therapist called ‘Thiele stripping’. A trigger point is found which when stimulated results in a twitch in the muscle underneath. A circular motion is exercised and then a pressure is applied to relax it. Internal massage helps release nerves.
- External massage techniques include skin rolling, deep tissue massage, trigger-point therapy to release tight spots, joint mobilization and nerve release.
In a study reported by WHO, instructions to women in pelvic floor muscle training (PMFT) has helped in both prevention and treatment of pelvic floor disorders in postpartum women.
Surgery: For Pelvic floor disorder that occurs due to rectocele or rectal prolapse, surgery is done to correct the condition.
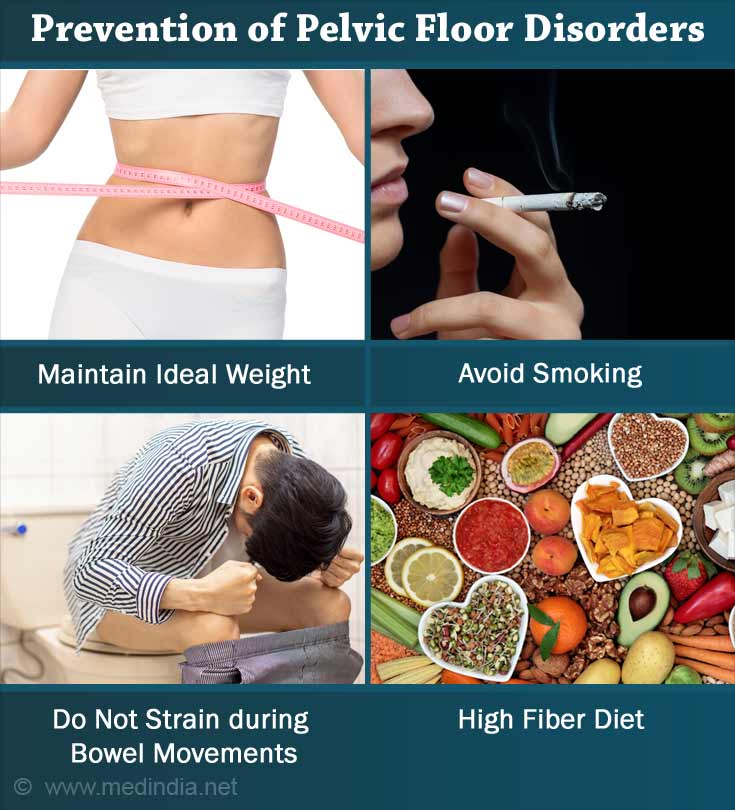
Prevention of Pelvic Floor Disorders
Prevention of pelvic floor disorders is possible in the following ways:
- Maintain ideal weight and optimum health
- Avoid smoking
- Pelvic floor exercises are recommended for pregnant women. Women with high-risk of pelvic floor disorders can also prevent the pelvic organ prolapse with kegels.
- Do not strain during bowel movements.
- Do not perform repetitive strenuous activities.
- Maintain the correct posture while lifting heavy objects.
- High fiber diet can prevent constipation, resulting in less strain on the muscles of the pelvic floor.
Health Tips
- Maintain a healthy lifestyle with adequate exercise and sleep.
- Eat healthy, nutritious and fiber rich food for proper movements of the digestive system.
- Drink at least 3 liters of water every day.
- Avoid constipation. Go for immediate help if suffering from constipation.
- Exercise the pelvic floor muscles by doing kegels (for women) and other activities like sit-ups and Pilates.
- Avoid a chronic cough as it increases the pressure on the muscles of the abdomen and pelvic floor.