- Diabetes and dental health - (https://www.mouthhealthy.org/all-topics-a-z/diabetes)
- Diabetes and Oral Health: Summary of Current Scientific Evidence for Why Transdisciplinary Collaboration Is Needed - (https://www.frontiersin.org/articles/10.3389/fdmed.2021.709831/full)
- Diabetes, Gum Disease, & Other Dental Problems - (https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/gum-disease-dental-problems)
- Oral health: A window to your overall health - (https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475)
- Your Diabetes Care Schedule - (https://www.cdc.gov/diabetes/managing/care-schedule.html)
About
Diabetes affects around 34 million in the United States. An estimated 210,000 youth and children under 20 years of age are diagnosed every year, according to studies.
Diabetes can have an adverse effect on your dental health. Learn how to protect your teeth and gums, and how good dental hygiene can also improve your overall health(1✔ ✔Trusted Source
Diabetes and dental health
Go to source).
Diabetes and Dental Health
The risk factors for diabetes include old age, obesity, family history of diabetes, prior history of gestational diabetes, impaired glucose tolerance (IGT), physical inactivity, and race/ethnicity.
Most people affected by this disorder should know that it can harm their eyes, heart, kidneys and blood vessels.
- Oral health problems are more likely to develop if the blood sugar level is uncontrolled along with poor oral hygiene.
- Glucose Helps Bacteria Multiply: The growth of certain bacteria existing in our oral cavity is controlled by the body’s natural defense mechanism and saliva to maintain a good oral hygiene.
- Uncontrolled diabetes that weakens the body’s main defense: The white blood cells against bacterial infections that occur in the mouth raises the glucose levels in saliva and this in turn facilitates the excessive growth of these bacteria.
- Plaque Formation & Gum Disease: These bacteria along with food taken form a soft, colorless, and sticky film known as plaque on the tooth surfaces, causes gum disease, bad breath, and tooth decay.
Recently, severe gum disease also known as periodontal disease is recognized as the "sixth complication" of diabetes mellitus(2✔ ✔Trusted Source
Diabetes and Oral Health: Summary of Current Scientific Evidence for Why Transdisciplinary Collaboration Is Needed
Go to source).
What are the Oral Health Problems Associated with Diabetes?
Dental Caries (Tooth Decay)
Decreased saliva production and increased sugar level in saliva seen in diabetic patients favor the growth of decay causing bacteria present in the mouth. This can lead to Dental caries or cavities.
Gum Disease
It is also known as periodontal gum disease, and stands as the most frequent and severe oral complication linked to diabetes.
Left untreated, this condition progresses through various stages, ranging from gum inflammation to eventual tooth loss. Elevated blood glucose levels heighten the risk of gum disease advancing from a mild to a severe state.
Gingivitis (Inflamed Gums)
The initial phase of gum disease is gingivitis, characterized by a mild inflammation of the soft tissues surrounding the teeth.
Gingivitis arises due to the accumulation of plaque and tartar near the gum line, leading to irritation and inflammation of the gums. Consequently, the gums may appear red, swollen, and prone to bleeding.
Periodontitis
When left untreated, gingivitis can evolve into periodontitis, an infection affecting the gums and the bone supporting the teeth.
The gums may recede from the teeth, forming pockets that gradually become infected. This commences the breakdown of bone and tissue holding the teeth in place and leads to bone loss. Without treatment, teeth can become loose and may require removal(3✔ ✔Trusted Source
Diabetes, Gum Disease, & Other Dental Problems
Go to source).
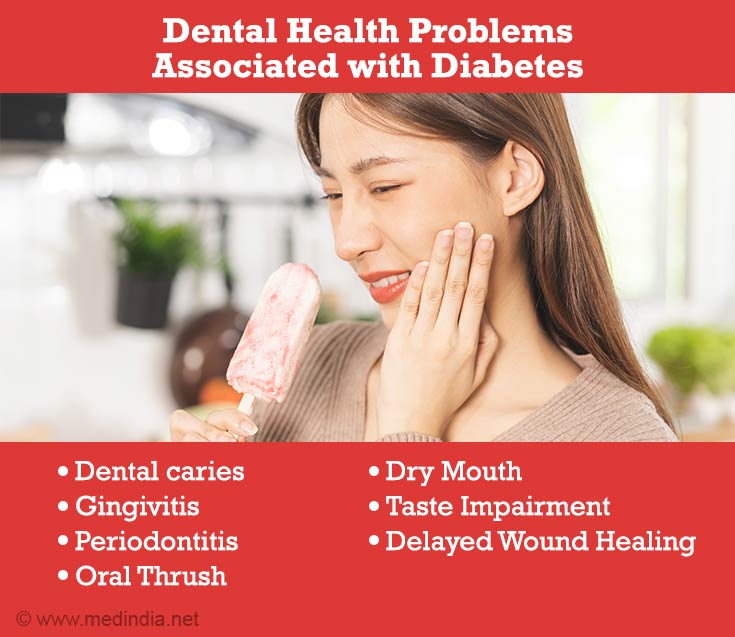
Oral Thrush
Also known as oral candidiasis. Diabetic patients taking antibiotics frequently to fight various infections are more prone to develop a fungal infection of the mouth and tongue.
The fungus thrives on the high glucose levels in the saliva of people with uncontrolled diabetes. Constantly wearing dentures can also lead to fungal infections.
Oral thrush produces white or red patches in the oral cavity that may transform to ulcers with pain, and burning sensation.
This condition is non-communicable and can be effectively managed using antifungal medication. If left untreated, the fungus can proliferate to other body parts, resulting in more severe complications.
Dry Mouth
Also known as xerostomia, a condition in which the mouth is abnormally dry.
Decreased saliva (spit) flow, oral sensory dysfunction, dehydration and altered saliva composition in diabetes can result in dry mouth. Dry mouth can further lead to soreness, ulcers, infections, and tooth decay.
Taste Impairment
Taste sensation can be influenced by the occurrence of peripheral neuropathy in diabetes. This sensory dysfunction inhibits the ability to maintain a proper diet and can lead to poor glycemic control and development of obesity.
Burning Mouth and/or Tongue
Diabetic patients are characterized by a bilateral burning sensation of the oral mucosa called burning mouth syndrome. This condition is caused by the presence of thrush and dry mouth.
Poor Healing of Oral Tissues
People with uncontrolled diabetes do not heal quickly after oral surgery or other dental procedures because of damaged blood flow to the treatment site. Diabetes often accompanies reduced immune function, which can negatively impact oral health.
Diabetes leads to a deficiency in cytokines. These proteins and lipids are crucial for the signaling and proper functioning of the immune system(4✔ ✔Trusted Source
Oral health: A window to your overall health
Go to source).
How to Prevent Oral Health Problems in Diabetic Patients?
On a Daily Basis
- Monitoring Blood Sugar: Follow your doctor's guidance and perform blood sugar checks as instructed, which may involve multiple checks throughout the day.
- Follow Dental Hygiene Methods: Use dental floss at least once a day to prevent plaque build-up on teeth. Brush your teeth after every meal using a soft-bristled toothbrush. Remove and clean your dentures once a day.
- Inspecting Your Feet: If you are unable to see the soles of your feet, use a mirror or seek assistance from a family member. Promptly inform your doctor if you notice any cuts, redness, swelling, sores, blisters, corns, calluses, or any other changes in your skin or nails.
- Adhering to Diabetes Medication: Take the prescribed dose of your diabetes medication as directed by your doctor, even when you are feeling well.
- Engaging in Physical Activity: Strive to engage in at least 150 minutes of moderate physical activity per week, such as brisk walking or cycling.
- Adopting a Healthy Diet: Consume nutritious foods that provide the required nutrients and assist in maintaining your blood sugar within the target range. Drink plenty of water and avoid consumption of sugary drinks.
Every Three Months
- A1C Test: If there have been alterations in your treatment plan or if you encounter difficulties in achieving your blood sugar objectives, undergo an A1C test every three months.
- Medical Checkup: If you encounter challenges in attaining your treatment goals, schedule a doctor's appointment every three months. During these visits, your blood pressure and weight will be assessed, your self-care plan and medications will be reviewed.
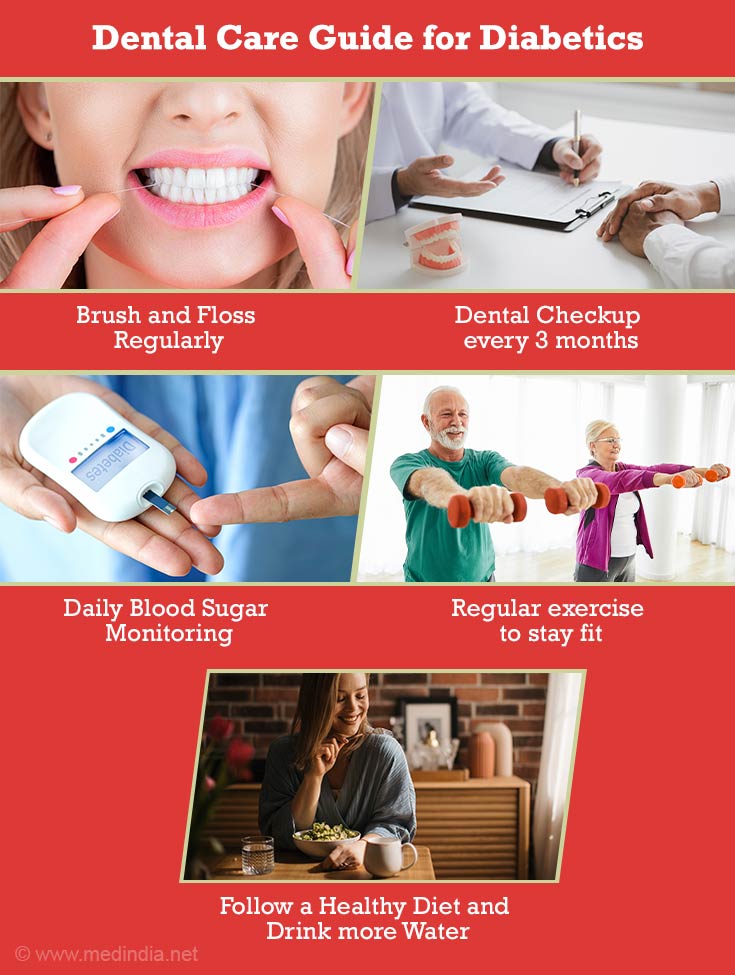
Every Six Months
- Dental Examination: Ensure you have your teeth and gums cleaned at least once a year, or more frequently if recommended by your doctor. Inform your dentist about your diabetes.
- Medical Checkup: For individuals meeting their treatment objectives, visit the doctor every six months.
Annually
- Influenza Vaccination
- Kidney Screening
- Cholesterol Profile
- Comprehensive Eye Examination (The frequency of this eye examination may need to be increased if you have diabetes-related eye issues).
- Hearing Assessment
- Thorough Foot Examination (The frequency of this foot examination may need to be increased if you have a history of diabetes-related foot problems).
As Necessary
- Mental Health Assessment: Promptly inform your doctor if you are experiencing feelings of sadness or hopelessness to receive appropriate assistance.
- New Symptoms or Health Issues: If you detect new health problems in early stages or if existing issues are worsening, contact your doctor immediately for evaluation(5✔ ✔Trusted Source
Your Diabetes Care Schedule
Go to source).
Prioritize Dental Care
Individuals with diabetes should prioritize their dental care by practicing good oral hygiene, including daily flossing and regular professional cleanings. This proactive approach to dental health is crucial because diabetes can increase the risk of oral health issues. Combining these practices with appropriate medical treatment can help maintain a healthy smile and overall well-being for those managing diabetes.


















