- The Pathogenesis and Natural History of Type 1 Diabetes - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3543105/)
- Diabetes Screening, Diagnosis, and Therapy in Pediatric Patients With Type 2 Diabetes - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2562149/)
- Treating type 1 diabetes - (http://kidshealth.org/en/parents/treating-type1.html?wt.ac=ctg#)
- Environmental Triggers of Type 1 Diabetes - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3385937/)
What is Type 1 Diabetes in Children?
Type 1 diabetes (T1D) also known as juvenile diabetes is one of the most common endocrine and metabolic disorders among children. Many studies also show that the rate of new cases diagnosed in many countries is highest among younger children. In type 1 diabetes, the pancreas loses the ability to produce insulin.
Insulin is normally produced by the beta cells of the islet of Langerhans that are present in the pancreas. After a meal, blood glucose levels increase. The pancreas then secrete insulin that helps cells absorb the glucose to use them for various metabolic processes. In type 1 diabetes, the body’s immune system attacks and destroys its own beta cells, thus causing a dearth of insulin and ultimately leading to disturbed glucose levels in the body.

What are the Causes and Risk Factors of Type 1 Diabetes in Children?
The exact cause of juvenile diabetes is unknown but researchers have so far identified two main factors:
- Genetics - Type 1 diabetes in children is perceived as a chronic immune-mediated disease. It results from an autoimmune destruction of insulin-secreting pancreatic β cells. The scientists suggest that the HLA genes explain approximately one-half of the genetic susceptibility for this disease.
- Environmental Triggers- Studies suggest that environmental stresses (specifically childhood obesity) increase insulin demand, thereby overloading islet cells and accelerating β-cell damage.
- Viral infections have also been implicated in the etiology of T1D. Enteroviruses, rotavirus or other either may have a cytotoxic effect or trigger an autoimmune process leading gradually to β-cell destruction.
- Dietary Factors- Early introduction of cow's milk proteins has been found to be a subsequent risk of β-cell autoimmunity and clinical disease. The American report also suggests that both early and late exposure to cereals is associated with an increased risk of β-cell autoimmunity. According to a Diabetes Prediction and Prevention project (DIPP) study, early introduction of fruits and berries as well as of roots is associated with increased risk for advanced β-cell autoimmunity.
The risks of acquiring type 1 diabetes are -
- Being a child (either 4-7 years old or 10-14 years old)
- Having a parent or sibling with the same
- Exhibiting certain genes
- Residing far away from the equator (in places like Finland and Sardinia)
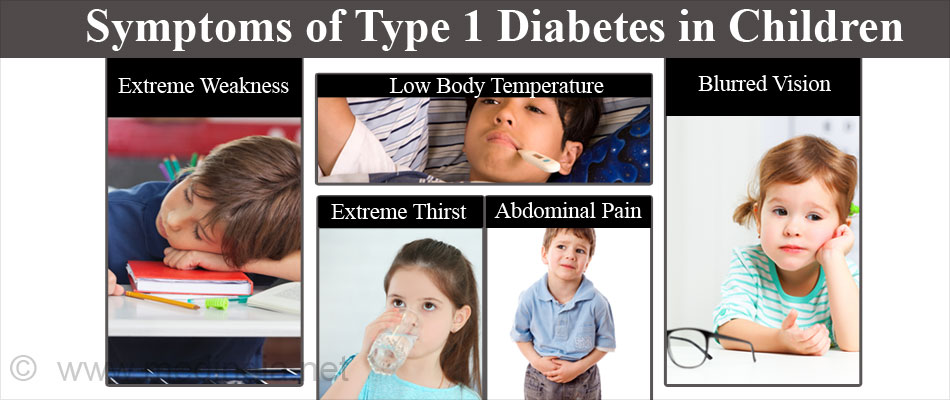
What are the Symptoms of Type 1 Diabetes in Children?
Type 1 diabetes develops gradually, however, its symptoms are seen suddenly. The signs & symptoms include:
- Extreme weakness and/or tiredness
- Increase in hunger
- Extreme thirst—dehydration
- Excessive urination
- Abdominal pain
- Blurred vision
- Wounds that don't heal well
- Weight loss - despite eating more
- Low body temperature (below 97º F)
How do you Diagnose Type 1 Diabetes in Children?
The criteria for screening of Type 1 diabetes in children include:
Overweight - A Body Mass Index (BMI) > 85th percentile for age and sex; or weight for age, sex, and height > 85th percentile; or weight > 120% of ideal height
In addition to any two of the following risk factors:
- Family history of type 2 diabetes in first or second-degree relative
- Signs of insulin resistance or conditions associated with insulin resistance, such as hyperpigmentation of the skin (acanthosis nigricans), hypertension, increased trigyceride levels, polycystic ovary syndrome
- Early puberty - age for initiation of screening is onset of puberty or 10 years
The primary test used to diagnose type 1 diabetes in children:
- Random Blood Sugar Test - A blood sample is taken at a random time. Blood sugar values are expressed in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). A random blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes.
- Glycated Hemoglobin (A1C or HbA1c) Test - This blood test indicates an average blood sugar level for the past 2-3 months. In this test the percentage of blood sugar attached to hemoglobin is measured.
HbA1c serves as a marker for average blood glucose levels over the previous three months before the last measurement as this is the lifespan of red blood cells. An A1C level of 6.5 percent or higher indicates diabetes.
- Fasting Blood Sugar Test - A blood sample is taken after an overnight fast. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. If it's 126 mg/dL (7.0 mmol/L) or higher on two separate tests, the child is diagnosed as diabetic.
What are the Complications of Type 1 Diabetes in Children?
Type 1 diabetes is associated with both short-term and long-term complications. The long-term complications mainly include:
- Cardiovascular problems
- Nerve damage or neuropathy
- Kidney damage
- Eye damage
- Skin problems
Type 1 diabetes is not preventable. The immunosuppressant drug, Cyclosporin might can halt destruction of beta cells in the latent autoimmune stage. However, Cyclosporin intake is associated with a lot of side effects.
Latest research suggests that an antimalarial drug called Artemisinin can transform glucagon producing alpha cells in the pancreas to insulin producing beta cells. It may have a potential as a therapeutic for diabetes in the future.
What are the Treatment & Management Methods for Type 1 Diabetes in Children?
Effective management & treatment for type 1 diabetes in children begins by establishing the goals of care. It includes blood sugar monitoring, insulin therapy, healthy eating and regular exercise. Currently, there is no cure for diabetes, so kids with type 1 diabetes need treatment for the rest of their lives. Following a proper treatment plan may help kids to stay healthy.
1. Monitoring Blood Sugar Levels
Treating type 1 diabetes involves checking blood sugar levels regularly and responding to the results. It helps kids with diabetes to grow and develop normally, and may also reduce the risk of long-term diabetes complications. In general, kids with type 1 diabetes should be tested for their blood sugar levels with a blood glucose meter at least four times a day. Another blood sugar test, the glycosylated hemoglobin (hemoglobin A1c or HbA1c) test should also be performed.

2. Insulin Therapy
Depending on your child's age and needs, the doctor may prescribe a mixture of insulin types to use throughout the day and night. The types of insulin available are:
- Rapid-acting Insulin- This starts working in five to 15 minutes and peaks about an hour after injection.
- Short-acting Insulin - This starts working about 30 minutes after injection and generally peaks in two to four hours.
- Long-acting Insulin - Ithas almost no peak and may provide coverage for as long as 20-26 hours.
- Intermediate-acting Insulin- It starts working 30 minutes to an hour after it has been taken and peaks in 4-6 hours.
Insulin Delivery Options
Often insulin is injected using a fine needle and syringe; but there are other options as well. There are tips to administer insulin effectively in children depending on what works best for your child. Conventional insulin administration involves subcutaneous injection with syringes marked in Insulin units. A few other alternatives are also available, like insulin pens and pumps. Shots given via insulin pens are a less expensive route and require less education and training compared to the computerized insulin pump. On the other hand, a pump offers more flexibility because it continuously delivers insulin and only requires one needle stick every 2-3 days when the site is changed.
- Insulin Pens - Insulin pens contain a cartridge of insulin that is inserted into the pen or there are pre-filled insulin pens which are discarded after all the insulin has been used.
- Insulin Pumps - Insulin pumps help to manage diabetes by delivering insulin 24 hours a day through a catheter placed under the skin.

The patient’s injection technique should be reviewed by a physician or diabetes educator. Painful injections can be minimized by adopting following steps:
- Inject insulin at room temperature. Injecting insulin in the same general area may give the best results from your insulin. Regular insulin works best if taken 30 minutes before eating.
- Make sure no air bubbles remain in the syringe before injection.
- Wait until topical alcohol (if used) has evaporated completely before injection.
- Keep muscles in the injection area relaxed, not tense, while injecting.
- Do not change direction of the needle during insertion or withdrawal.
- Do not reuse needles.
3. Healthy Eating
The best eating plan for a diabetic child includes avoiding sugary foods and incorporation of more green vegetables, fruits & whole grains.
4. Regular Exercise
Regular exercise increases the rate of absorption from injection sites, probably by increasing blood flow to the skin and also through local actions.
Health tips
In general, kids with type 1 diabetes should take care of following points:
- Take insulin as prescribed
- Eat a healthy & balanced diet
- Check blood sugar levels several times a day
- Get regular physical activity









