- Thymus Cancer - MedlinePlus, U.S. National Library of Medicine - (https://medlineplus.gov/thymuscancer.html)
- Thymus Gland Tumours - Cancer Research UK - (http://www.cancerresearchuk.org/about-cancer/thymus-gland-cancer)
- Thymus Cancer - American Cancer Society - (https://www.cancer.org/cancer/thymus-cancer.html)
- Thymus Gland Cancer - We are Macmillan. Cancer Support - (https://www.macmillan.org.uk/information-and-support/thymus-cancer)
- Thymoma and Thymic Carcinoma Treatment - National Cancer Institute, National Institutes of Health, USA - (https://www.cancer.gov/types/thymoma/patient/thymoma-treatment-pdq)
- Thymoma and Thymic Carcinoma - Cleveland Clinic - (https://my.clevelandclinic.org/health/articles/6196-thymoma-and- thymic-carcinoma)
- Thymus Cancer - Pacific Thymus Center, Pacific Heart, Lung & Blood Institute - (http://www.phlbi.org/divisions/lung-disease/thymic-cancer/)
- Tseng Y-L. Thymic carcinoma: a rare cancer requiring special attention. Formos J Surg 2011; 44(4): 136-40.
- Rashid OM, Cassano AD, Takabe K. Thymic neoplasm: a rare disease with a complex clinical presentation. J Thorac Dis 2013; 5(2): 173-83. DOI: 10.3978/j.issn.2072-1439.2013.01.12.
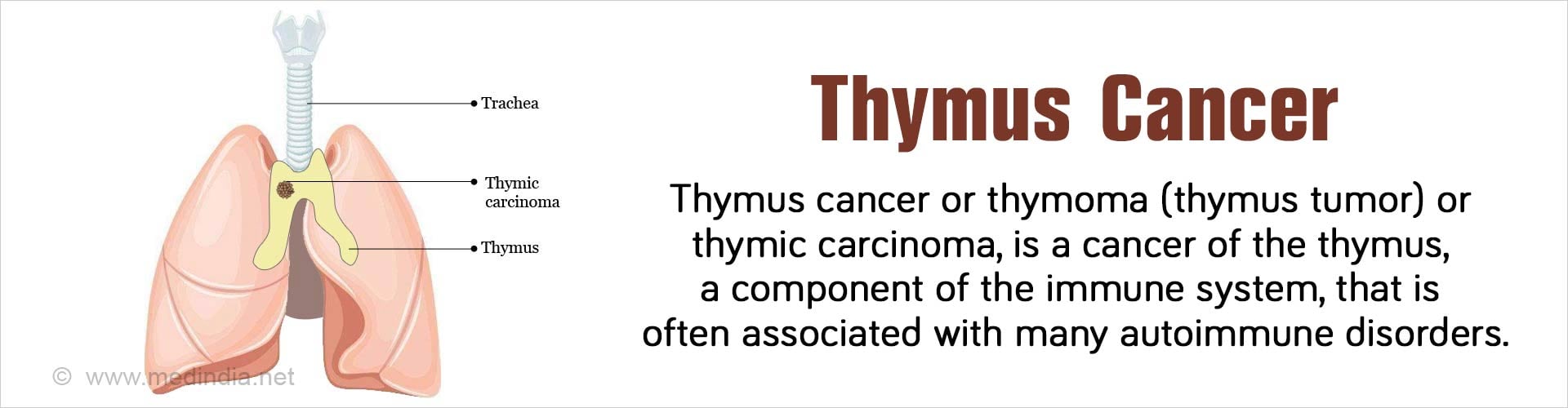
What is Thymus Cancer?
Cancer of the thymus gland is known by various names. Commonly it is simply referred to as thymus cancer. Alternatively, it is also called malignant thymoma (meaning thymus tumor) or thymic carcinoma. Earlier, tumors of the thymus were divided into benign (non-cancer) thymomas and malignant (cancer) thymomas. However most experts now believe that all thymomas turn malignant over time.
Thymus cancer is relatively rare, slow-growing tumors, and found mostly in people between the ages 40 to 60 years. The cancer cells develop on the outer lining cells of the gland (epithelial cells) and have the potential to spread to the lungs by a process called metastasis. It usually does not spread to other parts of the body.
Anatomy & Physiology of the Thymus Gland
The thymus is a small lymphoid organ that is concerned with formation of lymphocytes, a type of white blood cell. It is located in the neck and consists of two identical lobes and is located just behind the breast bone or sternum in the front part of the chest. The thymus is present in the mediastinum, the space between the two lungs, which houses the heart, part of the aorta, the food pipe or esophagus and a part of the wind-pipe or trachea. The thymus sits just in front and slightly above the heart. It produces T-lymphocytes or T-cells (T for “thymus”), which are active cells of the immune system – the body’s defense system, which attacks foreign invaders such as microbes that enter the body. These include potentially deadly pathogens such as bacteria, viruses, and fungi. The thymus tends to degenerate and become much smaller after reaching adolescence. However, the T-cells are produced throughout adult life, although at slower rates.
Epidemiology
Thymic cancer is very rare. According to statistics 1 in 1.5 million persons develops thymic cancer. With increasing use of computed tomography (CT) scan the numbers could be increasing.
WHO Classification of Thymus Cancer
The World Health Organization (WHO) has developed a system of classification for thymus cancer based upon the appearance of the cancer cells under the microscope (histology) into the following types: A, AB, B1, B2, B3, and C. Type AB and B2 are the most common, while type A is the least common. Progression of the cancer from type A to C means that the prognosis (outlook) gradually worsens.
What are the Causes of Thymus Cancer?
Very little is known about what causes thymus cancer. However, scientists have found that abrupt changes (mutations) in the DNA (deoxyribonucleic acid) – (the components of genes that carry information for protein production and function) – could be responsible. Importantly, why these mutations occur in some people and not in others, has still not been determined. However, some risk factors have been identified, which include the following:
- Age: The risk of thymus cancer increases with age.
- Ethnicity: Thymus cancer is most common in Asians and inhabitants of the Pacific islands and least common is white people and Latin Americans.
Association of Thymus Cancer with other Diseases
Thymus cancer can be linked with the following conditions, many of which are due to immune deficiency:
- Myasthenia gravis
- Systemic lupus erythematosus (SLE)
- Rheumatoid arthritis
- Pernicious anemia
- Hemolytic anemia
- Agranulocytosis
- Pure red cell aplasia (PRCA)
- Hypogammaglobinemia
- Cushing syndrome
- Nephrotic syndrome
- Ulcerative colitis
- Sarcoidosis
- Scleroderma
- Polymyositis
- Hypopituitarism
What are the Symptoms & Signs of Thymus Cancer?
Symptoms can occur from compression of adjacent structures due to cancerous growth. The structures that can be affected include the blood vessels, windpipe, and food pipe, all of which are located within the mediastinum. Symptoms include the following:
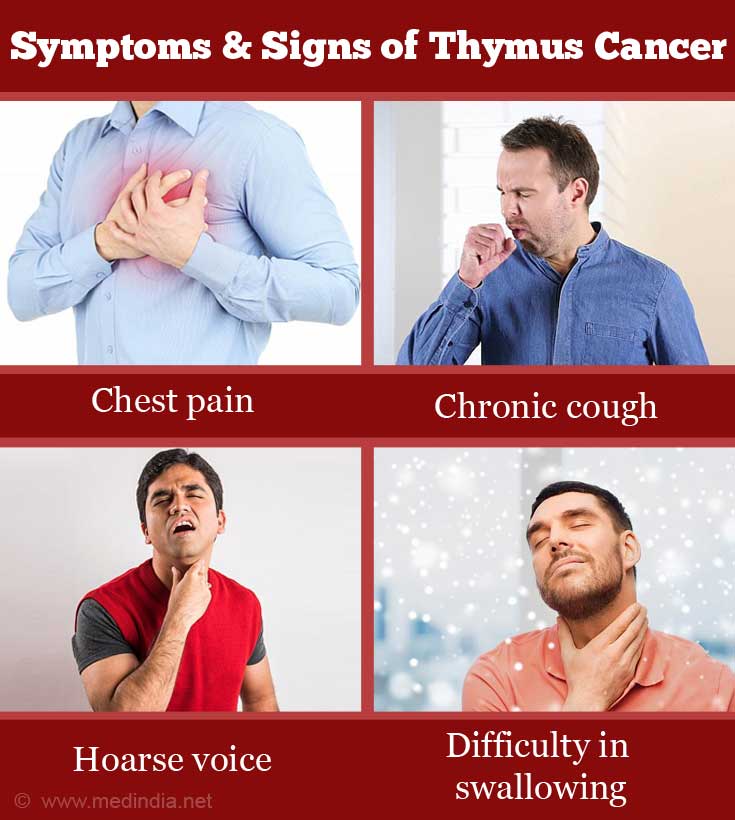
- Chest pain (due to acute pericarditis/myocarditis)
- Chronic cough (sometimes with blood tinged material discharged from airways)
- Superior vena cava syndrome
- Hoarse voice
- Difficulty breathing (dyspnea)
- Difficulty swallowing (dysphagia)
- Loss of appetite
- Tiredness
How do you Diagnose Thymus Cancer?
Diagnosis of thymus cancer is carried out in a stepwise fashion, which include the following:
- Medical History: The doctor will take a detailed history of the patient’s health habits, past illnesses, treatments, and hospitalizations (if any).
- Physical Exam: A thorough physical examination will be carried out by the doctor to assess if there are any abnormalities in the thymus such as swelling and/or pain. In case something is found to be wrong, imaging may be ordered.
- Imaging: Initially an X-ray will be ordered. This may be followed by a computed tomography (CT) scan which is a very accurate and sensitive imaging technique. A combination of CT with positron emission tomography (PET) i.e. CT-PET scan may be used to increase the sensitivity. Sometimes, magnetic resonance imaging (MRI) may be preferred because of its high accuracy.
- FNAC: Fine needle aspiration cytology (FNAC) involves obtaining cells by aspiration from the thymus using a fine needle. The samples as used for histologic studies. This technique is the ultimate confirmatory test because cancerous cells can be directly visualized, which is why it is considered the Gold Standard.
How do you Treat Thymus Cancer?
The common treatment modalities are briefly discussed below:
- Surgery: This is the most common treatment for thymus cancer. Surgery is used for removal or resection of the cancerous tissue from the thymus. Just in case any cancerous cells persist even after surgery, the patient is given radiotherapy, which is termed as adjuvant therapy.
- Radiotherapy: This uses high-energy X-rays or other types of radiation to kill the cancerous cells. Radiotherapy is of two types:
- External Radiotherapy: Here, the radiation is emitted from a machine outside the body and is focused on the area where the cancer is present. Thymus cancer is treated by external radiotherapy.
- Internal Radiotherapy: Here, a radioactive substance is placed within or adjacent to the cancerous tissue inside the body with the help of a needle, wire or catheter.
- Chemotherapy: This procedure uses various types of cytotoxic drugs such as cyclophosphamide, doxorubicin and cisplatin to either kill or stop the growth of cancer cells. A side-effect of chemotherapy is alopecia areata.
- Hormone Therapy: Hormones are substances secreted by hormonal (endocrine) glands that circulate via the blood and stimulate other organs. If any hormone is found to stimulate cancer cell division, drugs are used to block the hormone action. This is the basis of hormone therapy. Hormone therapy using drugs such as corticosteroids can be used to treat thymus cancer.
What is the Prognosis for Thymus Cancer?
The prognosis (outlook) for patients with thymus cancer depends on the following factors:
- Stage of the Cancer: If the cancer is in late stage, then the prognosis is poor.
- Cancer Type: Prognosis is best for type A and worst for type C.
- Patient’s Health: Prognosis is better in a healthy patient.
- Efficacy of Surgery: Prognosis is better if the tumor can be completely removed by surgery.
- Recurrence of Cancer: Prognosis is poor if the cancer comes back.