- Jefferson J, Rich P. Melanonychia. Dermatol Res Pract. 2012;2012:952186. - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3390039/)
- Mayo Clinic. Fingernails: Possible Problems. Accessed Aug 14, 2018. Cited Aug 14, 2018. Updated 2018. - (https://www.mayoclinic.org/healthy-lifestyle/adult-health/multimedia/nails/sls-20076131?s=5)
- Scheinfeld N, Dahdah MJ, Scher R. Vitamins and minerals: their role in nail health and disease. J Drugs Dermatol. 2007;6(8):782-787. - (https://www.ncbi.nlm.nih.gov/pubmed/17763607)
- Singal A et al. Subungual melanoma is not so rare: Report of four cases from India. Indian Dermatol Online J. 2017;8(6):471-474. - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc5707841/)
- Mole RJ, MacKenzie DN. Cancer, Melanoma, Subungual. [Updated 2018 Jan 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan. - (https://www.ncbi.nlm.nih.gov/books/nbk482480/)
- Bishop JN et al. The prevention, diagnosis, referral and management of melanoma of the skin: concise guidelines. Clin Med. 2007;7(3):283-290. - (http://www.clinmed.rcpjournal.org/content/7/3/283.full.pdf+html)
- Bristow IR et al. Clinical guidelines for the recognition of melanoma of the foot and nail unit. J Foot Ankle Res. 2010;3:25. - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2987777/)
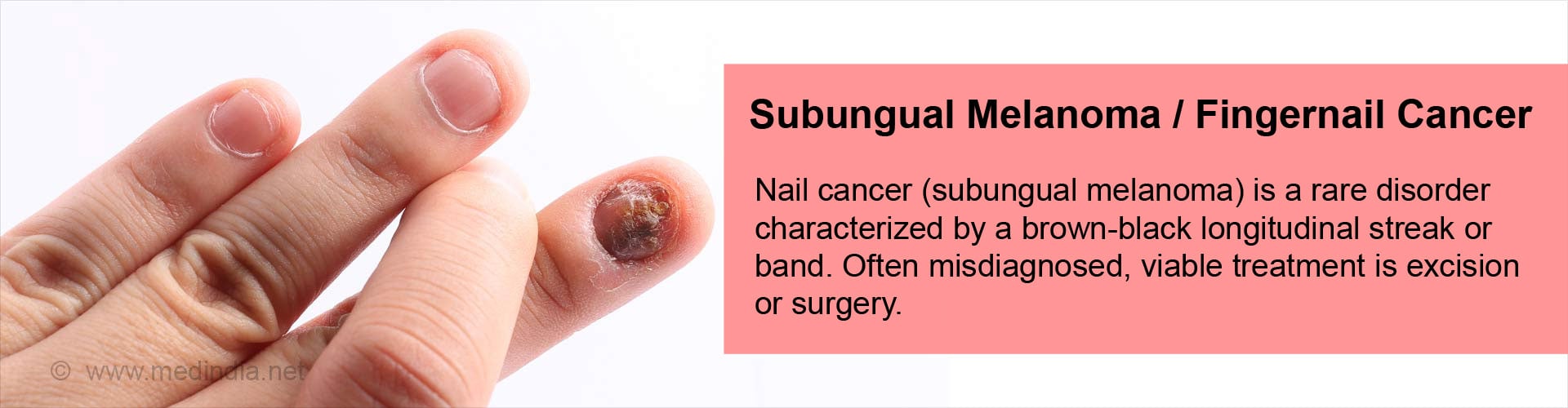
What is Subungual Melanoma?
Melanoma is skin cancer arising from skin melanocytes (melanin pigment-producing cells). Subungual (under the nail) melanoma is a rare skin cancer constituting 0.7% to 3.5% of all malignant melanomas. This form of cancer is a variant of acral lentiginous melanoma, a malignant cancer of the soles and palms. The toe and thumb are the most commonly affected (75% to 90%) digits in subungual melanoma.
Subungual melanoma develops as a brown-black pigmented band in the nail matrix and appears initially at the nail fold (edge of the nail with the skin). The band slowly widens and the growth tends to shift the nail from its position with concurrent bleeding. If detected early, the condition can be treated immediately with a good outcome (prognosis) and the cancer can be halted and even reversed.
Normally, men over 70 years and women over 60, are affected with subungual melanoma. Nearly 25% Chinese, 10% Japanese, 75% African-Americans, 33% Native Americans, 16% Mexicans, and 1%-3% Caucasians are affected with subungual melanomas rather than cutaneous melanomas, or cancers that start in the pigment-producing cells of the skin.
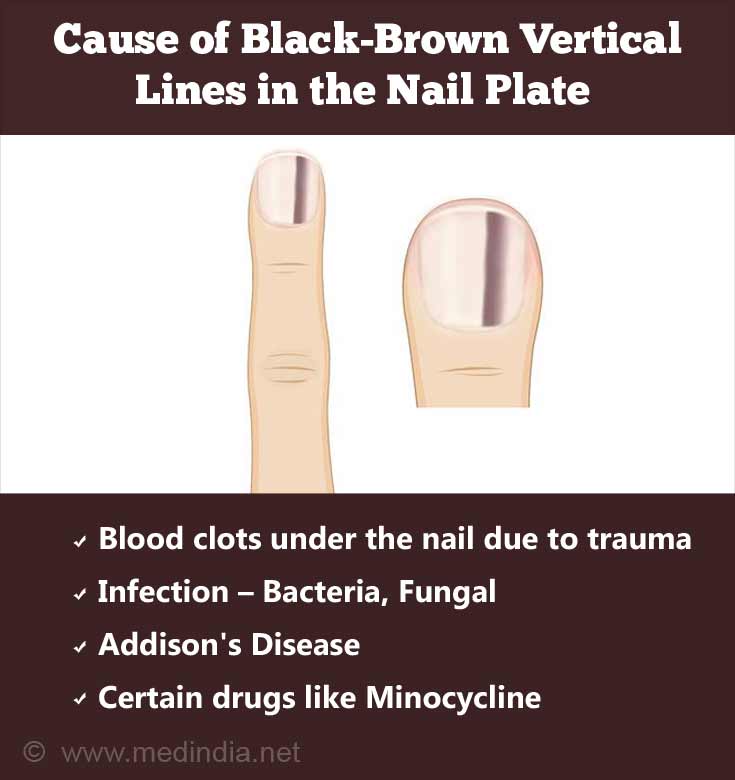
What are the Causes of Black-brown Vertical Lines in the Nail Plate?
Melanoma within the nail is a result of activated melanocytes that multiply in the nail matrix and begin to spread to the nail. The exact cause of melanoma is not known though ultra-violent radiation is a risk factor for its development. However, this may not be the cause for fingernail melanoma.
The cause of black-brown vertical lines in the nail plate that may mimic melanoma of fingernail include:
- Blood clots under the nail due to trauma
- Infection from - Bacteria, Fungal or HIV infection
- Certain drugs treatment for example Minocycline
- Addison's Disease
All the above are benign conditions and should not be confused with cancer or melanoma of the nail plate. If you are worried, please check with your doctor.
One should also remember that melanoma can affect the palms of the hands or the soles of the feet too and is more common in people with darker skin.
What are the Symptoms & Signs of Subungual Melanoma?
The initial signs of subungual melanoma are streaks or black-brown bands on the nail bed. The pigmentation may be irregular. Subsequently, the nail thickens, may split or is completely damaged resulting in swelling, pain, pus secretion and discoloration of the surrounding region.
A characteristic sign (Hutchinson sign) of subungual melanoma is the spread of melanin pigment from the nail to the surrounding skin.
What are the Consequences of Subungual Melanoma?
Subungual melanoma is invariably diagnosed late and so the 5-year survival rate ranges between 16% and 87% based on the stage of the cancer. With advanced stages, the survival rate drops. Different factors affect the survival rate of subungual melanoma, such as:
- Breslow thickness – A good survival indicator for subungual melanoma (lower the thickness of the tumor, better the survival rate).
- Tumor metastases – Distant metastases to the lymph node or liver
- Tumor stage
How do you Diagnose Subungual Melanoma?
Some of the risk factors considered in diagnosing subungual melanoma are compiled as ABCDEF guidelines. The guidelines are useful to identify lesions that need to be excised. The guidelines are:
- Ethnic origin and age – Chinese, Japanese, African-American or Native Americans are more susceptible to subungual melanoma.
- Black-brown band with irregular border (>3mm)
- Change in rate of growth and size or lack of improvement with treatment
- Digit – usually one affected digit, such as big toe, thumb, or index finger
- Extension of discolored pigmentation e.g. Hutchinson sign
- Family history of cases of melanoma is recorded<
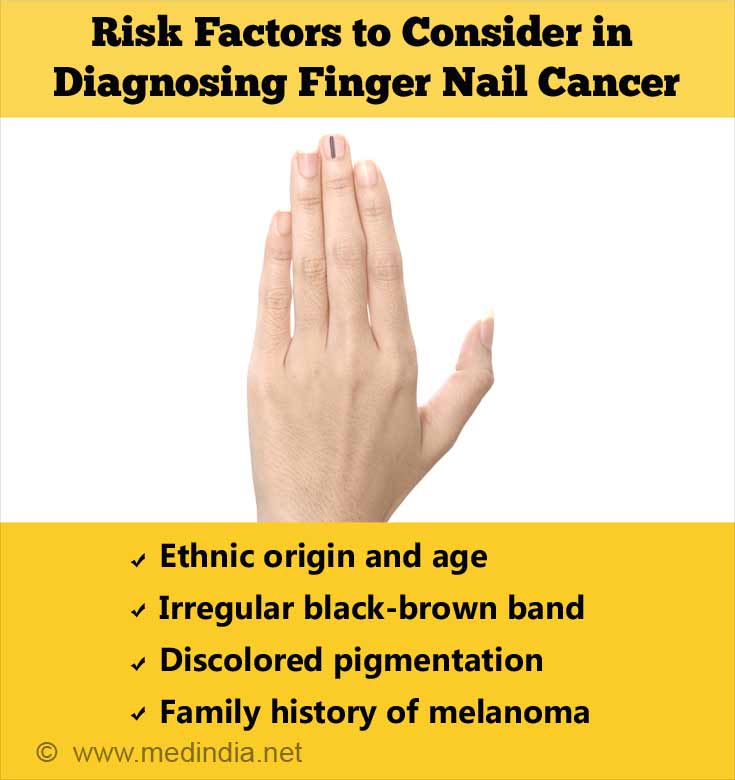
In order to accurately diagnose subungual melanoma, it is important to follow the above guidelines, compare the lesions with earlier photographic evidence, and immediately excise (cut out entirely) suspicious lesions. The tissue pathology of the nail shows an increased number of melanocytes. The metastatic cases exhibit a 2- to 3-fold increase in the number of melanocytes compared with benign cases.
Nail dermoscopy (onychoscopy) is a noninvasive method to differentiate between benign and advanced cases of cancer. It also confirms longitudinal melanonychia. However, intraoperative direct matrix dermoscopy is invasive and helps to determine if nail biopsy or excision is required.
There are 2 clear ways to confirm subungual melanoma.
- The pigmentation in melanoma arises in the nail matrix and nail fold. If the pigmentation develops in the nail bed with a normal nail matrix and nail fold, then the pigmentation is not considered a melanoma.
- If there is melanoma in the nail bed, then there is a history of melanoma originating in the nail matrix and nail fold.
How do you Treat Subungual Melanoma?
Most often, subungual melanoma is misdiagnosed as infection due to a hematoma (swelling due to blood clot), a fungal infection, trauma, or a mole on the skin. This affects the survival outcome.
Basic treatment of subungual melanoma involves tumor excision. Initially, an excision nail biopsy helps to diagnose the condition. When the cancer becomes invasive, amputation is the preferred option. Often, the extent of excision is determined by the tumor’s Breslow thickness. Digit-sparing amputation improves survival rate and reduces recurrence.
Lymph nodes, if they are palpable, should be analyzed with imaging. Biopsy may or may not be carried out. If the disease is identified, lymph nodes need to be dissected. Lymph node biopsies are performed on lesions that are 1mm to 4 mm in thickness. If the thickness exceeds 4 mm, brain MRI scans and CT-PET imaging is used to stage the tumor.
Immunotherapy and radiotherapy are utilized only in specific cases. Radiotherapy is used on lymph nodes with large lymphadenectomy.
How to Prevent Subungual Melanoma?
Unfortunately, subungual melanoma is always diagnosed in the late stages. Ideally, patients and family physicians should be vigilant and try to diagnose the condition early. If the pigmentation does not respond to traditional forms of treatment, a dermatologist should be consulted to avoid the condition from progressing to the advanced stage.
Close inspection and vigilance are very important in recognizing subungual melanoma with the least amount of delay.