- Share Psychotic Disorder - (http://www.disorders.org/personality-disorders/shared-psychotic-disorder/)
- Share Psychotic Disorder - Individual Cases - (https://en.wikipedia.org/wiki/Folie_%C3%A0_deux#Individual_cases)
What is Shared Psychosis Disorder?
Shared psychosis disorder also referred to as folie a deux is a rare mental illness in which an otherwise normal and healthy person starts to believe the delusions (false beliefs) of a closely connected person such as spouse, sibling or friend who has a psychotic disorder like schizophrenia, for example.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-4) classifies shared psychotic disorder (folie à deux) as an atypical psychotic disorder. A diagnosis of an atypical psychosis is made when a patient shows symptoms that are clearly psychotic such as delusions (false beliefs), hallucinations (seeing and hearing things that don’t exist), disorganized thinking, thought broadcasting (the belief that one’s thoughts are broadcast from the head to the outside world) or other bizarre behaviors. However, these symptoms do not satisfy the level required by the DSM-5 to diagnose a specific psychotic disorder such as schizophrenia.
The person who has the psychotic disorder is the primary or dominant partner and the other person is referred to as the secondary or passive partner.
The primary or dominant partner and the passive partner often have a strong emotional connect to one another but are otherwise not very social and may not have other friends or acquaintances other than each other.
The dominant partner has a strong influence or hold over the passive partner and gradually manages to impose their false beliefs on the passive partner very soon. The primary member, usually older, more intelligent and better educated with an assertive personality, controls the passive member who is usually docile and weak.
Most often, this disorder occurs within a nuclear family; more than 95% of the cases reported were from members of the same family. A third of reported cases were between two sisters and another third being between mother and child and husband and wife.
Although shared psychosis disorders typically involve two persons, it can involve three persons (folie à trois), four persons (folie a quatre) and in case it affected 12 members of the same family (folie a famille/ folie á douze). It can also happen in a group or cult where the cult leader has a psychotic disorder and imposes his false beliefs on his followers (folie à plusiers, or "the madness of many").
Famous Cases of Shared Psychosis Disorder
Some of the reported interesting cases of shared psychosis disorder or folie a deux are given below in order to give an idea of the bizarre and almost unbelievable things that can happen in this condition.
Shared psychosis involving an entire family
In 2016, a bizarre case involving a family of five from Melbourne, Australia made the news when all of them suddenly disappeared from their home leaving everything behind and travelled more than 1,600 km across the state of Victoria because one of the family members was convinced that someone was out to kill them. Over the next few days, each person was found in a separate location in a confused state with no proper explanation as to how they reached there.Following an investigation by the police, no evidence was found to support the family’s claims of persecution and the symptoms of those involved resolved on their own once the family returned to their home.
Shared psychosis between an owner and her pet dog
Volume 149 of the American Journal of Psychiatry reports a case of folie a deux shared between an 83-year-old widow and her pet dog.
The woman had seriously believed that her upstairs neighbor was trying to make her flee her home.
She believed that he was harming her and her pet dog with “violet rays,” so she made the dog an “air raid shelter” under the kitchen table. Whenever the dog heard any noise from above, it would run and hide in its spot.
Whether this was a case of folie a deux or whether the dog was carrying out what its owner asked it to do remains unclear. However, whatever the dog’s real motivation may have been, it was still participating in its owner’s delusion.
Shared Psychosis between husband and wife
Margaret and her husband Michael, both aged 34 years, were both found to be suffering from folie à deux when they were both were found to share similar delusions that people were out to harm or persecute them. They believed that some persons were entering their home, “spreading dust and fluff and wearing down their shoes". Interestingly, both also had symptoms supporting a diagnosis of emotional contagion (see glossary), made separately in both of them.
Burari Deaths in India in June 2018
A family of eleven members from Burari, India committed suicide in June 2018 due to the shared delusion of one of the family members about mistakes committed and attaining salvation. One hypothesis put forward in this perplexing case is that shared psychosis disorder may have led to the deaths.
What are the Causes of Shared Psychosis Disorder?
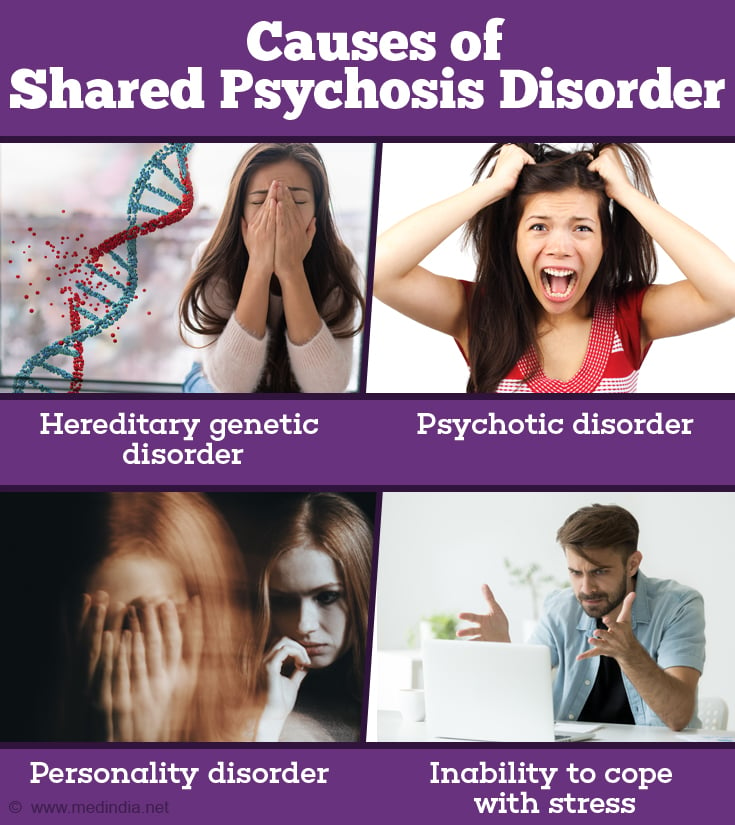
There is a complex combination of several factors involved, although the exact reasons are still not clear
- Since many of these cases involve members of the same family, there is a strong suggestion that there might be a genetic component in the development of this disorder
- The primary person has a diagnosable psychotic disorder
- The passive partner may have a family history of psychiatric illness in a first degree relative other than the primary partner
- The secondary partner may be suffering from a personality disorder that causes dependence or submission or he/she may be predisposed to mental illness
- Social isolation (total or partial lack of contact with society) of the family or persons involved
- Inability to cope with stress
- Other factors that can influence the development of shared psychosis disorder include the degree of closeness between the two persons, the duration of their relationship and the existence of dominant versus passive nature of the relationship
What are the Symptoms & Signs of Shared Psychosis Disorder?
- Presence of a dominant person with a psychotic disorder
- Often the delusions are believable and seem possible in comparison to some of the bizarre delusions that some schizophrenia patients have. It is thus easy to impose these delusions on the weaker person
- Firm and unshakeable belief by the passive partner in the dominant partner’s delusion

How do you Diagnose Shared Psychosis Disorder?
A family physician will take a detailed history and conduct a thorough physical examination. There are no specific tests to diagnose shared psychosis disorder and imaging tests such as CT or MRI of the brain may be advised to rule out any brain disease as the cause for the symptoms. If there is no cause found for the patient’s symptoms, a referral to a mental health professional or psychiatrist may then be made.
A clinical discussion with a mental health professional is necessary to diagnose shared psychotic disorder. The following criteria have to be satisfied to confirm the diagnosis of shared psychosis disorder
- Development of un-shakeable or firm delusion (false belief) in an otherwise normal and healthy person, living in close association with someone who already has known psychotic disorder
- The nature of the delusion is remarkably similar to the delusion in the primary person
- The delusion seen in the secondary person cannot be explained since they do not have any underlying psychotic illness such as schizophrenia
How can you Treat Shared Psychosis Disorder?
Treatment of shared psychosis disorder focuses on the passive partner. Treatment methods include the following
- Separation of the passive partner from the dominant partner
- Strong psychological and emotional support following the separation from the dominant partner to ease the distress. However, symptoms will ease once the passive person is removed from the unhealthy association
- Counseling and psychotherapy – This may aid in the promotion of healthy thinking, boosting one’s confidence and reduction of symptoms
- Family therapy – This involves the family of the affected person and urges them to support and encourage the person’s interests and development of social ties and be regular with medication
- Anti-psychotic medications – They may be used only if symptoms have not significantly improved following conservative treatment measures
For the primary partner, treatment usually involves antipsychotic medications and psychotherapy. If the primary partner is considered to be a physical threat to others, the person may be hospitalized until this is no longer the case.

How do we Prevent Shared Psychosis Disorder?
In order to prevent relapse or recurrence of the condition, continued family therapy should also be considered to modify old and unhealthy family dynamics. Social and community support may also help since the family cannot continue to exist in isolation as previously as it did in the past.