- Information About Psoriatic arthritis - (http://www.arthritisresearchuk.org/arthritis-information/conditions/psoriatic-arthritis.aspx)
- Overview - Psoriatic arthritis - (http://www.nhs.uk/conditions/psoriatic-arthritis/pages/introduction.aspx)
- Psoriatic Arthritis - (http://www.rheumatology.org/i-am-a/patient-caregiver/diseases-conditions/psoriatic-arthritis)
- More on Psoriatic arthritis - (http://www.mayoclinic.org/diseases-conditions/psoriatic-arthritis/home/ovc-20233896)
- About Psoriatic Arthritis - (https://www.psoriasis.org/about-psoriatic-arthritis)
- What is Psoriatic Arthritis? - (http://www.arthritis.org/about-arthritis/types/psoriatic-arthritis/what-is-psoriatic-arthritis.php)
What is Psoriatic Arthritis?
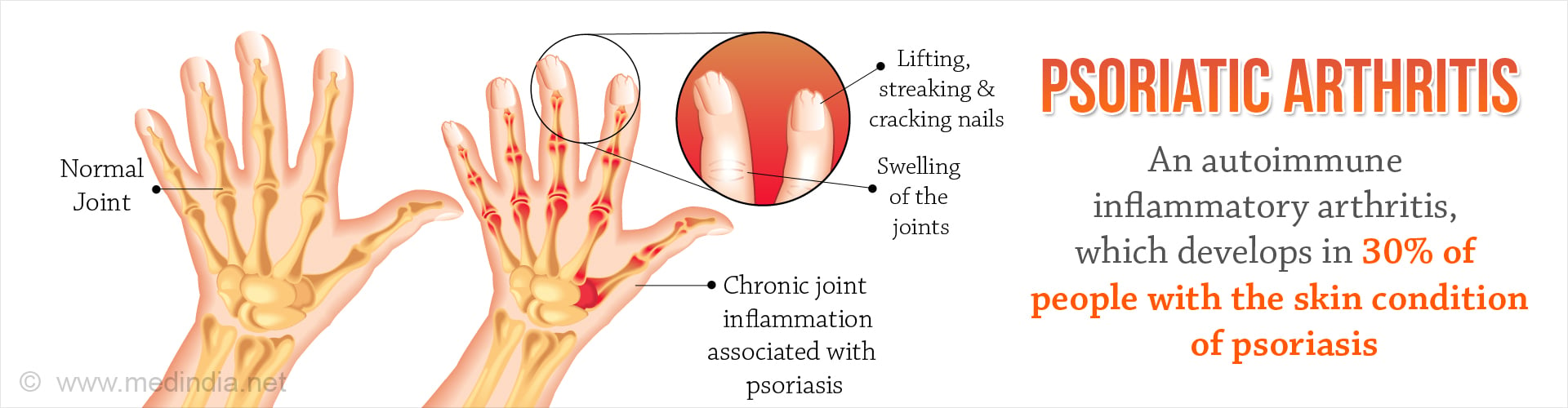
Psoriatic arthritis is a kind of autoimmune inflammatory arthritis, which develops in 30 percent of people with the skin condition of psoriasis. Psoriasis is a skin condition that causes a red rash, topped with silvery scales, typically on the elbows, knees, back, hips, and scalp.
Psoriasis affects people of any age, both male and female; however, psoriatic arthritis usually affects more adults as compared to the young people.
Psoriatic arthritis is a long-term condition that can get progressively worse. The disease might lay dormant in your body unless it is triggered by some outside force, like a common throat infection or bacterial infection. Delaying the therapy for psoriatic arthritis by as little as six months could result in permanent joint damage and the patient might require surgical treatment in such cases. However, with early diagnosis and adequate treatment, it is possible to retard the progression of the condition and prevent permanent damage to the joints. Most of the patients develop psoriasis initially and are diagnosed later with psoriatic arthritis; but in some cases, the joint problems might begin prior to the appearance of skin lesions. In both psoriasis and psoriatic arthritis, disease flaring might alternate with intermittent periods of remission.
Psoriatic arthritis is an autoimmune disease and it occurs when our immune system unknowingly attacks our own healthy tissues, which are the joints and skin in this case. The hampered immune response triggers inflammation, causing the affected joints to become inflamed (swollen), stiff and painful. Symptoms of psoriatic arthritis can be been experienced in any part of your body, including the fingertips and spine, and it usually ranges from relatively mild to extreme cases. The joints are permanently damaged in extreme cases. Psoriasis patients might also have other types of arthritis, such as osteoarthritis or rheumatoid arthritis, but these are not necessarily linked to psoriasis.
What are the Types of Psoriatic Arthritis?
Based on the involvement of joints there is
- Symmetric psoriatic arthritis- It constitutes fifty percent of cases of psoriatic arthritis. It affects joints on both sides of the body at the same time just like in case of rheumatoid arthritis.
- Asymmetric psoriatic arthritis- It constitutes thirty-five percent cases of psoriatic arthritis. It does not appear in the same joints on both sides of the body at the same time.
- Oligoarticular- It is the mild form of disease and it affects four or fewer joints in the body.
- Polyarticular- It is the severe form of disease and it affects four or more joints
Based on the location of the joints involved there is
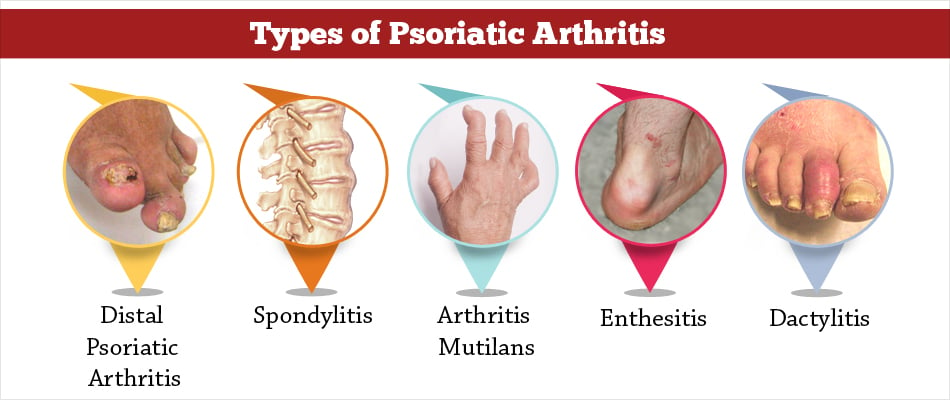
- Distal psoriatic arthritis - It causes inflammation and stiffness near the ends of the fingers and toes, along with certain changes like pitting, white spots, and lifting from the nail bed.
- Spondylitis - It refers to inflammation of the spinal cord. Pain and stiffness in the spine and neck are hallmarks of this form of psoriatic arthritis.
- Arthritis mutilans - It is the most severe form of psoriatic arthritis and it affects 5 percent of people. It causes deformities in the small joints of the fingers and toes, and can destroy them.
- Enthesitis - Entheses is the site where ligaments or tendons insert into the bones. Enthesitis refers to the inflammation of entheses. Common locations are the bottoms of the feet, the Achilles' tendons, and the margins where ligaments attach to the ribs, spine, and pelvis. It is exclusively a type of psoriatic arthritis and never manifests in other forms of arthritis like rheumatoid arthritis or osteoarthritis. It causes the tissues in the affected area to become ropey (known as fibrosis) or solid (known as ossification or calcification).
- Dactylitis - It is also known as "sausage digits," and it refers to inflammation of an entire finger or toe. Dactylitis is another exclusive type of psoriatic arthritis. Dactylitis involves a few fingers and/or toes, but not in a symmetrical pattern.
What are the Causes and Risk Factors of Psoriatic Arthritis?
The single greatest risk factor of developing psoriatic arthritis is having psoriasis. One to two of every five patients with psoriasis develop psoriatic arthritis; it develops within 10 years of diagnosis of psoriasis. The causes and other risk factors are as follows:
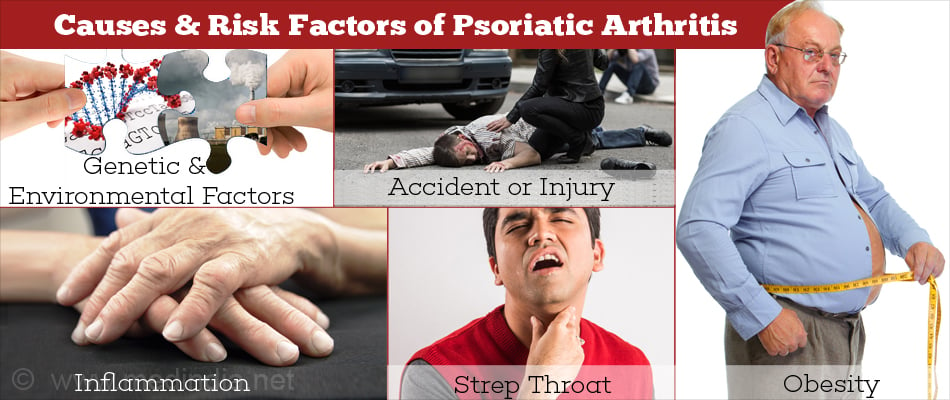
- Psoriatic arthritis is the result of the immune system mistakenly attacking healthy tissues of its own body. Both genetic and environmental factors play a role.
- The arthritis is caused by inflammation. The process of inflammation is almost similar in the skin and the joints. A particular combination of genes makes some people more susceptible to develop psoriasis and psoriatic arthritis. An infection might act as a trigger in people who are already at risk of this type of arthritis, for example bacteria that live in patches of psoriasis. Psoriasis is not infectious; however, the disease may be triggered by a strep throat.
- Sometimes the disease might follow an accident or injury, particularly if it affects a single joint.
- Obese people are more at risk of developing both psoriasis and psoriatic arthritis.
- A family history of either psoriasis or psoriatic arthritis makes the person more susceptible. Approximately forty percent of patients have family members affected by the disease.
What are the Symptoms of Psoriatic Arthritis?
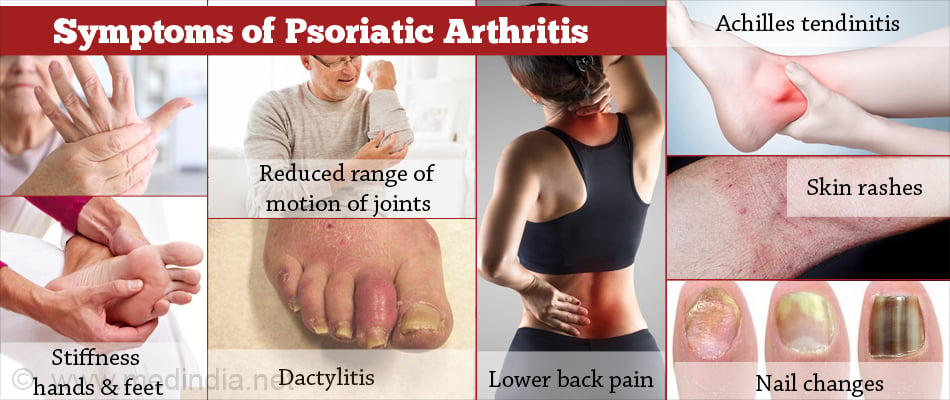
- Pain, swelling and, stiffness that can affect any joint in the body, most commonly in the hands & feet, knees, neck, spine and elbows. The severity of the condition varies from person to person. It can affect joints on just one side or on both sides of the body.
- Joints that are warm to touch.
- Reduced range of motion of joints.
- Remission periods when your symptoms improve.
- Flare ups or relapses when symptoms get worse.
- Dactylitis is a sausage-like swelling along the entire length of fingers or toes and occurs due to inflammation in both joints and tendons. It is a feature unique to psoriatic arthritis and helps to differentiate psoriatic arthritis from rheumatoid arthritis (RA).
- Lower back pain that includes buttock pain, a stiff back, or a stiff neck due to inflammation in your spine; the condition is known as spondylitis, a form of inflammatory arthritis.
- Foot pain that causes pain and swelling at the back of your heels, where the Achilles tendon attaches to the bone. This condition is known as Achilles Tendinitis. It may also cause pain in the sole of foot and the condition is known as plantar fasciitis.
- Skin rashes that appear as thick, red skin with flaky, silver-white scaly patches.
- Nail changes likepitting, discoloration and thickening of nails. The nail separates from the nail bed, becomes pitted, and mimics fungus infections. The skin and nail changes are unique to psoriasis and psoriatic arthritis and helps the doctors confirm a diagnosis.
- Fatigue is common.
- Morning stiffness of joints.
- Eye problems like inflammation of the eyes, which causes redness, irritation, disturbed vision, and pain in tissues surrounding the eyes.
- Diarrhea and gastrointestinal problems. Psoriatic arthritis is closely linked with Crohn’s disease.
- Lung problems like a condition known as interstitial lung disease, which manifests as shortness of breath, coughing, and fatigue.
How do you Diagnose Psoriatic Arthritis?
Symptoms of psoriatic arthritis vary among different people. Many of the symptoms are common to other forms of arthritis and hence diagnosis is difficult. Psoriatic arthritis may closely mimic rheumatoid arthritis, gout, and osteoarthritis, making it mandatory to perform differential diagnosis for each of them.
There are no specific tests for psoriatic arthritis. The diagnosis is based on patient’s symptoms and physical examination. The doctor will compulsorily check for psoriasis and must ask for history of psoriasis or psoriatic arthritis in patient’s family.
Certain tests that can be employed are:
- Blood tests that check for signs of inflammation and the presence of certain antibodies found in other types of arthritis.
- X-rays to rule out other types of arthritis, such as rheumatoid arthritis and osteoarthritis.
- Rheumatoid factor (RF): RF is an antibody found in the blood of people with rheumatoid arthritis. It is absent in the blood of people with psoriatic arthritis thereby helping to differentiate both the conditions.
- Joint fluid test: Uric acid crystals found in the joint fluid indicates the presence of gout rather than psoriatic arthritis.
What is the Differential Diagnosis of Psoriatic Arthritis?
Symptoms of psoriatic arthritis can be similar to other conditions. For example, patients of both rheumatoid and osteoarthritis also have general feelings of fatigue.
In addition, waxing and waning of symptoms which manifests as periods of increased disease activity and symptoms, is also a common feature of various types of arthritis. Also, a common feature of both psoriatic arthritis and rheumatoid arthritis is joint pain in the morning or after a brief period of rest.
Hence, it is very important to know key features of similar conditions to differentiate them from psoriatic arthritis.
- If only a single joint swells up rapidly and there is intense pain that probably lasts overnight it is gout.
- If there is little or no joint swelling, with pain especially after an activity the diagnosis is most likely osteoarthritis.
- Symmetrical joint pain that affects the same joint on both sides of the body is indicative of rheumatoid arthritis as opposed to psoriatic arthritis that is asymmetrical and affects only one side of the body.
How do you Treat Psoriatic Arthritis?
There is no specific cure for psoriatic arthritis; the focus is on controlling symptoms and preventing damage to the affected joints. One of the aims of the treatment is to slow down the progression of the condition and improve the quality of patient’s life.
The main medications used to treat psoriatic arthritis are:
1. Nonsteroidal anti-inflammatory drugs (NSAIDs):
- Ibuprofen
- Naproxen
- Diclofenac
- COX-2 inhibitors (often called coxibs), such as celecoxib or etoricoxib
A medication called a proton pump inhibitor (PPI) is prescribed alongside NSAIDs to combat the side effects of NSAIDs.
2. Corticosteroids:
Corticosteroids help reduce pain and swelling. Medication is directly injected if you have a single inflamed or swollen joint. This causes rapid relief with minimal side effects. They can also be taken as a tablet. However, it can cause significant side effects if used in the long term, and psoriasis might flare up on stopping the drug abruptly instead of slow tapering off and then discontinuing.
3. Disease-modifying anti-rheumatic drugs (DMARDs):
These ease the symptoms and slow the progression of psoriatic arthritis. The earlier a DMARD is started, the more effective it will be. Examples are:
- Leflunomide: (It is the first drug given for psoriatic arthritis).
- Sulfasalazine
- Methotrexate
It usually takes several weeks or months for a DMARD to start working, so you must continue taking the medication, even if it does not seem to be working at first.
4. Biological treatments:
Biological drugs stop particular chemicals in the blood from activating the immune system so they stop attacking the cells of our own joints. Examples include:
- Adalimumab
- Apremilast
- Certolizumab
- Etanercept
- Golimumab
- Infliximab
- Secukinumab
- Ustekinumab
5. Other modalities of treatment:
- Physiotherapist: Gives advice on exercises to help maintain the mobility.
- Occupational therapist: Gives advice on protecting the joints from further damage. They might use splints or train you to alter the way you perform tasks to reduce the strain on the affected joints.
- Podiatrist: Assesses the foot care needs and offers advice on special footwear.
- Treatments for the skin: Ointments are used. There are five main types of ointments:
- Tar-based ointments
- Ointments made from a medicine called Dithranol
- Steroid-based creams and lotions
- Vitamin D-like ointments such as Calcipotriol and Tacalcitol
- Vitamin A-like (retinoid) gels such as Tazarotene
If the creams and ointments do not help with psoriasis, following options are available:
- Light therapy (also called phototherapy) in which, exposure to high-intensity ultraviolet light is carried out in hospital
- Retinoid tablets
- Methotrexate tablets or injections
How can you Prevent and Manage Psoriatic Arthritis?
Early recognition, diagnosis, and adequate treatment of psoriatic arthritis can help prevent or limit extensive joint damage. Patients with psoriasis must regularly be screened for symptoms of joint trouble.
Avoid straining your finger joints by rough handling of objects, if you are a patient of psoriasis. Maintain a healthy weight, this will help to put less strain on your joints. Eat more plant-based foods — fruits, vegetables and whole grains.
Do regular exercises, like biking, swimming, and walking which can help keep your joints flexible and your muscles strong. Take rest before you become too tired to avoid fatigue. Divide exercise or work activities into short segments.

Health Tips
Psoriasis patients must be sure to tell their doctor if they develop joint pain. If left untreated, it can severely damage the joints.