- Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)–Patient Version - (https://www.cancer.gov/types/lymphoma/hp/mycosis-fungoides-treatment-pdq#section/all)
- Mycosis fungoides - (https://ghr.nlm.nih.gov/condition/mycosis-fungoides)
- Shujaa A, Suriya MO. Mycosis Fungoides Presentation in Emergency. The Open Emergency Medicine Journal, 2011, 4, 17-21
- Akinbami et al. Mycosis Fungoides: Case Report and Literature Review. Clinical Medicine Insights: Case Reports 2014:7 95–98 doi: 10.4137/CCRep.S15724
- Mat Samuji M.S and Gilmore J. Mycosis Fungoides Tumour. International Journal of Clinical & Medical Imaging. 2016; 3 (4): 100045 http://dx.doi.org/10.4172/2376-0249.1000458
What is Mycosis Fungoides?
Mycosis fungoides is a type of cutaneous T-cell lymphoma, a cancer caused by abnormal proliferation of a type of white blood cells called T lymphocytes or T-cells and their infiltration into the skin.
The first thought that comes to one’s mind on hearing the words mycosis fungoides is that it is probably a fungal infection. The mushroom-like appearance of the lesions prompted Baron Jean-Louis Alibert, who first described the condition in 1806, to give the cancer its name. The discovery that mycosis fungoides was caused by T-cells came much later. In fact, the term cutaneous T-cell lymphoma for cancers like mycosis fungoides came into use only in 1975.
Mycosis fungoides is more specifically, a cancer of CD4 T lymphocytes (T cells that have a CD4 glycoprotein on their surface), which play an important role in maintaining immunity. The cancerous cells localize in the skin causing the skin lesions, but are not present in the blood. Mycosis fungoides is the most common type of cutaneous T-cell lymphoma. The other common type is Sézary syndrome, where the cancerous cells are found in the skin as well as the blood. Some regard Sézary syndrome as a late stage of mycosis fungoides.
What are the Causes of Mycosis Fungoides?
Like for most other cancers, the exact reason why mycosis fungoides affects only certain people is not known. Mycosis fungoides probably arises due to a combination of:
- Genetic factors: People with mycosis fungoides have been found to have genetic changes like additions of DNA in regions of chromosomes 7 and 17 or loss of DNA in regions of chromosomes 9 and 10, which can arise during the lifetime of the individual. However, it is not clear if these are responsible for the development of the cancer. Certain variants of the HLA class II genes may also predispose to mycosis fungoides.
- Environmental factors: People working in the paper processing, glass, pottery and ceramics industries appear to be at a higher risk.
- Infection with the human T-cell leukemia virus 1 (HTLV-1) virus. Infection with the HTLV-1 virus, which spreads through sexual contact, intravenous drug use or breastfeeding, could play a role in the development of mycosis fungoides, though this has not been confirmed.
Factors that increase the risk for developing mycosis fungoides include the following:
- Gender. The condition affects males twice more commonly as compared to females.
- Age of individual between 45 to 60 years, though it has also been diagnosed in younger people as well.
- Race. Blacks are affected more commonly than Whites and Asians.
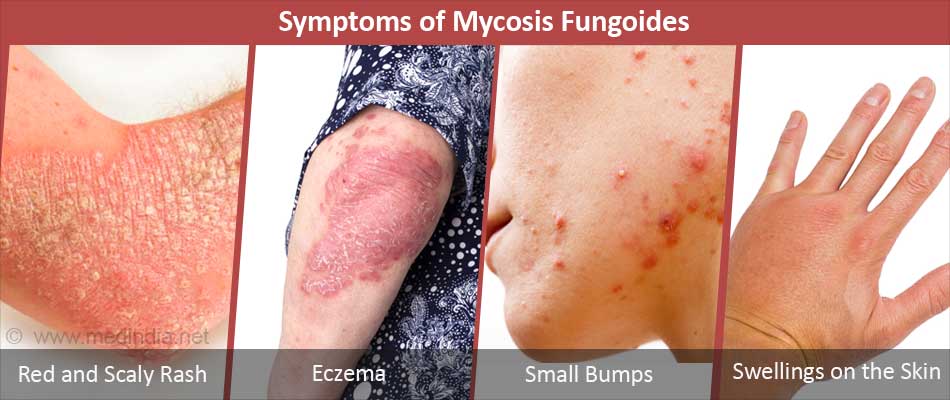
What are the Symptoms of Mycosis Fungoides?
Mycosis fungoides evolves through several stages, which are evident from the skin changes:
- The premycotic phase is characterized by a red and scaly rash on parts of the skin that are not exposed to sunlight like the buttocks, inner thighs, back, and the breasts.
- The patch phase marks the appearance of thin, red lesions that appear like eczema.
- The plaque phase is characterized by small bumps or raised, thickened skin, which are often itchy. The patches and plaques may be lighter or darker than the normal skin color, or may show the presence of small red spots.
- The tumor phase, where swellings appear on the skin. The tumors may ulcerate or get infected.
Complications of mycosis fungoides include:
- Spread to other parts of the body such as liver, spleen, lymph nodes and lungs.
- Recurrence following initial treatment.
- Infection with dangerous bacteria like Staphylococcus aureus and Pseudomonas aeruginosa, which can result in blood infection or sepsis.
How do you Diagnose Mycosis Fungoides?
Diagnosis of mycosis fungoides, especially in the early stages, is extremely difficult since the features are similar to those of other skin conditions like chronic contact dermatitis, atopic dermatitis and psoriasis. It is therefore important for the examining doctor to keep in mind that such presentations could be due to mycosis fungoides.
The diagnosis of mycosis fungoides is made based on the following:
- History and physical examination of the skin lesions
- Blood tests, which may include the following:
- Blood counts and examination of a peripheral blood smear. Patients with Sézary syndrome will show abnormal blood counts
- Measurement of liver enzymes to check if the liver is affected
- Measurement of uric acid and lactate dehydrogenase levels to check for the disease aggressiveness
- Immunophenotyping, which uses special staining to differentiate blood cancer cells from normal cells
- T cell receptor gene rearrangement test, to check for genetic changes in the lesions
- Flow cytometry, which is used to study blood cells and identify the malignant clone
- HTLV-1 testing can be done to check for underlying infection
- Biopsies, which may include the following:
- Skin biopsy, where a small part of the skin lesion is cut out and examined under a microscope. This will show collections of the typical abnormal T-cells
- Lymph node biopsy on an enlarged lymph node to detect spread of the cancer
- Bone marrow biopsy to detect the presence of cancer in the bone marrow
- Imaging tests: Imaging tests like chest x-rays, CT scan, PET scan are used to detect spread of the cancer to inner organs
The TNMB (tumor-node-metastasis-blood) staging is used to identify the stage of the cancer. Staging helps the treating doctor to decide on the best treatment for the patient and the possible outcomes of the cancer. A later stage usually has a poorer prognosis.
How do you Treat Mycosis Fungoides?
Treatment for mycosis fungoides may be either local, systemic or a combination of these. Treatments include the following:
Photodynamic therapy: Two forms of photodynamic therapy are used in the treatment of mycosis fungoides:
- PUVA (psoralen and ultraviolet A) therapy. In this type of treatment, a drug called psoralen is injected into the body, which localizes into the cancer cells. Laser is then used to activate the drug within the cells. The procedure selectively kills the cancerous cells without affecting the normal cells.
- Extracorporeal photopheresis. In this procedure, some white blood cells are collected, treated with a photosensitizing medication, exposed to ultraviolet light, and then re-introduced into the body. The procedure is repeated several times.
Radiation therapy: Radiation therapy is given in the form of external beam radiation, or total skin electron beam (TSEB) radiation therapy which mainly targets skin cells, or ultraviolet B (UVB) radiation therapy using special lamps or laser.
Medications: Several chemotherapy drugs like topical Mechlorethamine, oral Methotrexate and PEGylated lysosomal Doxorubicin are used alone or in combination to treat mycosis fungoides. Other drugs that may be used in addition include the following:
- Corticosteroids to reduce inflammation
- Retinoids like Bexarotene, which are a form of vitamin A
- Biological treatments like interferons
- Denileukin diftitox which is produced from diphtheria toxin

Targeted therapy: Targeted therapy uses medications that precisely target cancerous cells without affecting normal cells, thereby reducing the side effects associated with the treatment. Targeted therapies used in mycosis fungoides include the following:
- Alemtuzumab
- Vorinostat
- Romidepsin
- Pralatrexate
Few localized lesions can be surgically removed. Stem cell transplantation is also being evaluated for mycosis fungoides







