- Intestinal Ischemic Syndrome - (https://my.clevelandclinic.org/health/diseases/17136-intestinal-ischemic-syndrome/follow-up-care)
- Bowel Ischaemia - (https://patient.info/doctor/bowel-ischaemia)
- Clinical Review: Mesenteric ischaemia - (https://www.gponline.com/clinical-review-mesenteric-ischaemia/gi-tract/article/1110549)
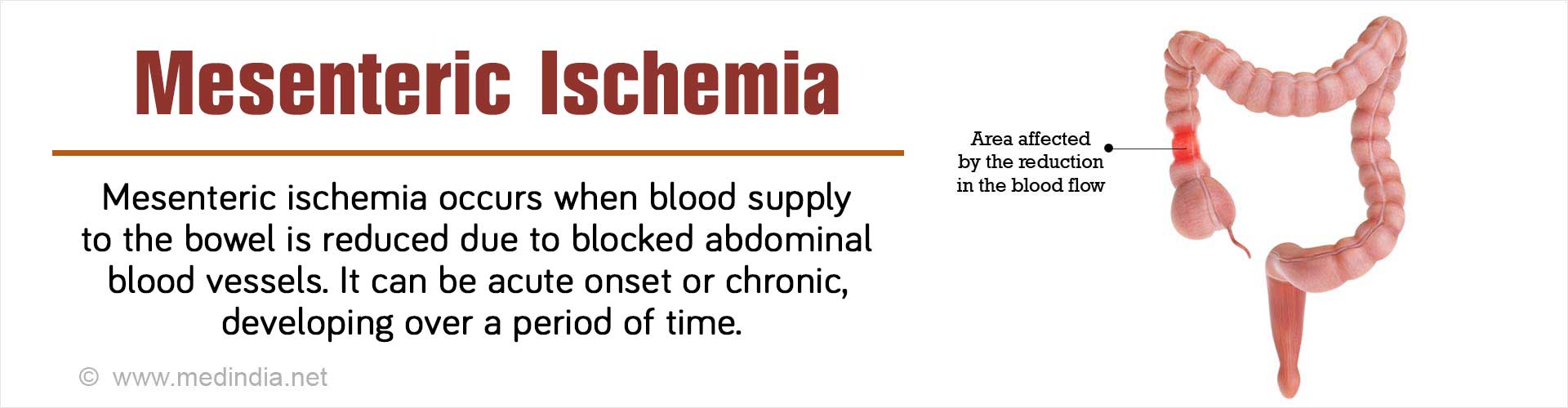
What is Mesenteric Ischemia?
Mesenteric ischemia refers to a group of disorders marked by decreased blood supply to the bowel due to blockage or narrowing of the blood vessels that supply them. It can occur suddenly without warning (acute mesenteric ischemia or AMI), which needs immediate surgery.
Less commonly, when the symptoms develop gradually over time it is described as chronic. Chronic mesenteric ischemia (CMI) is also termed intestinal angina. Unless treated chronic mesenteric ischemia results in severe weight loss and malnutrition or can become acute.
Overview of Blood Supply of Bowel
Mesenteric blood vessels refers to the blood vessels that carry blood to the small and large bowel. The three important abdominal blood vessels that may be affected include the celiac artery, superior mesenteric artery or inferior mesenteric artery. At least two of these arteries must be blocked or narrowed to cause intestinal ischemic syndromes.
Epidemiology of Mesenteric Ischemia
Mesenteric ischemia is quite rare and the overall prevalence is approximately 0.1% of all hospital admissions. It usually occurs in persons over 50 years but can affect younger persons with pre-existing risk factors such as atrial fibrillation.
What are the Causes of Mesenteric Ischemia?
The most common cause of mesenteric ischemia is when the blood vessels that carry blood to the small and large bowel become clogged with fat deposits and fibrous tissue. This will cut off or severely reduce blood flow to these organs causing abdominal pain and other symptoms.
| Acute Mesenteric Ischemia (Sudden onset and emergency) | Acute arterial occlusion or blockage (70% cases)
|
Non-occlusive mesenteric ischemia (NOMI) (20% cases)
| |
Mesenteric vein thrombosis (5-15%)
| |
Rare conditions
| |
| Chronic Mesenteric Ischemia (develops gradually over time) |
|
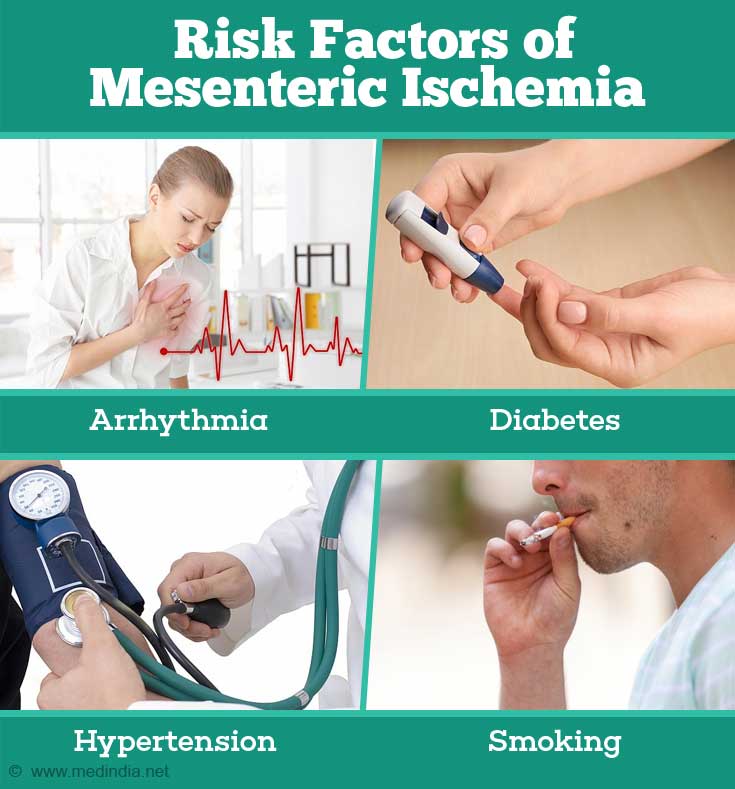
What are the Predisposing / Risk Factors of Mesenteric Ischemia?
As stated above, mesenteric ischemia is mainly caused due to atherosclerotic arterial disease. Thus, any factor which predisposes to atherosclerosis can be a risk factor for mesenteric ischemia. Risk factors and associations include
- Underlying heart disease - Myocardial infarction (heart attack), arrhythmia (atrial fibrillation), cardiomyopathy
- Diabetes (increased blood sugar levels)
- Hypertension (elevated blood pressure)
- Smoking history
- Hypercholesterolemia (increased blood cholesterol especially LDL-cholesterol)
- Peripheral arterial disease (blood vessel disease of lower limbs)
- Drug abuse
What are the Symptoms of Mesenteric Ischemia?
| Acute Mesenteric Ischemia (sudden onset and emergency)Symptoms tend to have a more gradual onset in NOMI and venous thrombosis |
|
| Chronic Mesenteric Ischemia (develops gradually over a time period) |
|

How do you Diagnose Mesenteric Ischemia?
If mesenteric ischemia is suspected, further diagnostic imaging to evaluate bowel and circulation systems will be necessary. Acute mesenteric ischemia is a life-threatening condition and prompt diagnosis and appropriate treatment is critical in saving the patient’s life.
- Blood Tests – May show increased white cell count (leukocytosis) and metabolic acidosis. Liver function tests, urea and electrolytes
- Stool Culture – May be useful to rule out acute infective diarrhea presenting with similar picture with acute abdominal pain
- Electrocardiogram (ECG) - May show evidence of atrial fibrillation or myocardial infarction
- Echocardiogram - This test is an ultrasound investigation of heart and is done to show the presence of heart abnormalities such as blocked coronary arteries, and presence of heart disease that may have caused mesenteric ischemia.
- Imaging Tests
- Abdominal x –ray: Can show characteristic findings such as dilation of the segments of intestine and air in the wall of the intestine. Sometimes the bowel wall may also give way and can be seen on an x-ray as a large amount of air under the dome of diaphragmatic muscle
- Chest x-ray – To rule out pneumonia
- Abdominal CT and MRI – May help rule out other causes of acute abdomen
- CT-Angiogram: The primary investigation of choice due to high sensitivity for diagnosing AMI (>90%).Contrast-enhanced magnetic resonance angiography (CE-MRA) is another option
- Mesenteric arteriogram – It is the gold standard to diagnose acute mesenteric ischemia but not used in the first instance as it is invasive. Contrast material is injected into the blood vessels and x-ray images are obtained to outline any narrowing or blockage
- Intraoperative fluorescein administration - May be useful to delineate those areas of bowel that need resection
How do you Treat Mesenteric Ischemia?
Acute Mesenteric Ischemia (AMI)
Patients with suspected AMI are initially stabilized with a combination of oxygen, IV fluids, antibiotics and heparin.
- Surgery - Emergency surgery is done to remove the blood clot (embolectomy) or bypass the narrowed/blocked vessel (revascularization) from the aorta or iliac arteries (autologous grafts) or artificial grafts in order to restore blood flow to the intestines. Non-viable and gangrenous segments of the bowel need to be excised (removed by cutting)
- Clot busting medications – In the absence of bowel perforation or peritonitis, or if the symptoms are less than 8 hours duration, an arteriogram may be done to visualize the mesenteric arteries and inject a clot busting drug to break down the clot (thrombolysis).
- Miscellaneous – In patients with non-occlusive mesenteric ischemia (NOMI), they should be given drugs to improve blood flow in the affected mesenteric vessel. Drugs used for this purpose are termed vasodilators and include papaverine, prostaglandin E1, and nitroglycerine.
Chronic Mesenteric Ischemia
Treatment for chronic mesenteric ischemia is important to reduce the risk of blood clot formation and prevent further intestinal damage. Treatment options include:
- Medication - Anticoagulants such as Coumadin (warfarin - a blood-thinner) is given to reduce the risk of blood clots. Patients on warfarin have to be monitored regularly.
- Angioplasty and stenting - A balloon catheter is inserted and inflated to attempt to widen the artery and a small stent is placed inside the artery to keep it open.
- Surgery may be performed to remove atherosclerotic plaque (transaortic endarterectomy), bypass the blocked vessel using grafts (revascularization) to restore blood flow to the intestines, or remove or repair an aneurysm. The grafts may be autologous bypass grafts (patient’s own blood vessels) or artificial grafts during the bypass procedure.
What is the Prognosis of Mesenteric Ischemia?
In acute mesenteric ischemia which is a medical emergency, mortality rates remain high. This is mainly due to not making an early diagnosis based on clinical suspicion since several conditions present in a similar manner with sudden severe stomach pain. By the time investigations are done and a definite diagnosis is made, the affected part of small bowel is permanently damaged with complications. A delay of 24 hours in treatment can reduce survival by 20%. Thus early diagnosis and treatment is key for better patient outcome in acute mesenteric ischemia.
Chronic mesenteric ischemia has a good prognosis, with a five-year survival rate of 70%.Studies have shown graft patency up to 78% at five years with traditional open surgical vascular bypass procedures, while angioplasty and stenting (endovascular procedures) are associated with medium-term success rates of >90%, but may require repeat procedures.
In either case, survivors of extensive bowel resection are looking at a lifetime of disability.