- Harrison's Textbook of Medicine 19th edition
- What is Acute Liver Failure? - (http://www.nejm.org/doi/full/10.1056/nejmra1208937#t=article)
- Definition - Acute Liver Failure - (http://www.mayoclinic.org/diseases-conditions/liver-failure/basics/definition/con-20030966)
- Acute Liver Failure - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2933761/)
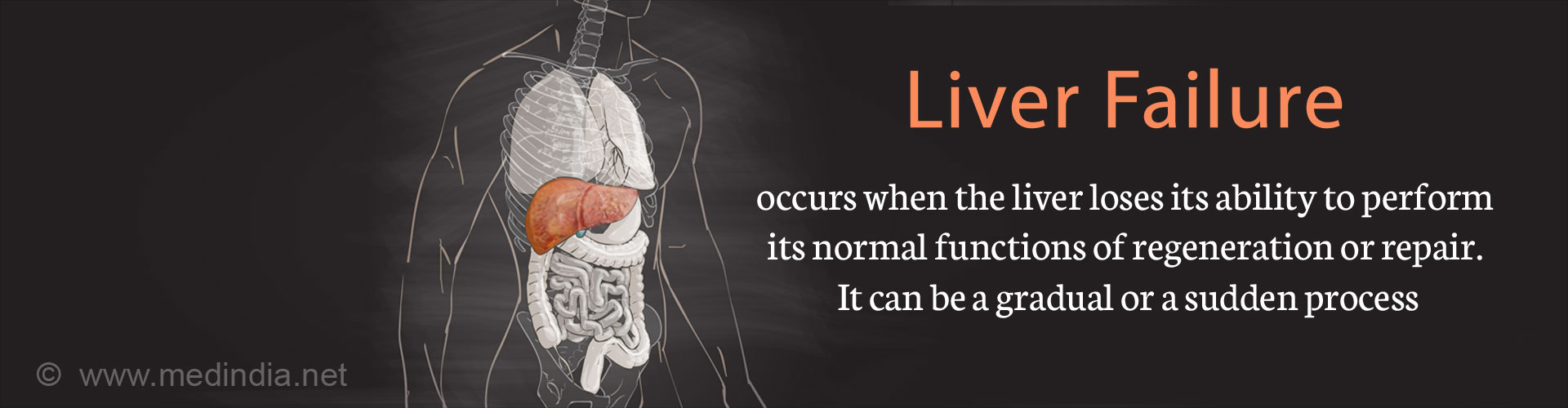
What is Liver Failure?
Liver failure occurs when the liver has lost its functional abilities. Liver failure can be acute or chronic. Another form that is being recognized nowadays is acute-on-chronic liver failure.
What is the Anatomy of the Liver?
The liver is a dark, reddish-brown organ situated in the upper right-hand portion of the abdominal cavity. The oxygenated blood supply comes to the liver via two kinds of blood vessels. 25% of blood flows into the liver through the hepatic artery and the remaining 75% of nutrient-rich blood flows into the liver through the hepatic portal vein.
The liver consists of two main lobes, both of which are formed by eight small segments, which in turn are made up of a thousand lobules. These lobules unite and connect to small ducts that in turn connect with larger ducts to eventually form the common hepatic duct.
What are the Types of Liver Failure?
Liver failure is categorized into three distinct groups:
- Acute liver failure (ALF): In acute liver failure the loss of liver function develops quickly within days or weeks most commonly in a patient who has no evidence of pre-existing liver disease. It can lead to serious life-threatening complications within 4 weeks, which includes excessive bleeding (coagulopathy) and elevated brain pressure (intracranial pressure). It is a medical emergency, which requires immediate hospitalization.
- Chronic liver failure (CLF) occurs due to cirrhosis (where normal tissue is replaced by scar tissue); cirrhosis could inturn be caused by different liver diseases.
- Acute-on-chronic liver failure (ACLF): This occurs to someone who develops features of liver failure when already having chronic liver disease. Alcohol misuse or infection could be a cause. These patients might become critically ill and require intensive care treatment, and maybe a liver transplant.
What are the Causes of Liver Failure?
1. Acute Liver Failure
- Chronic infections by viruses such as Hepatitis viruses (A, B and E), Epstein-Barr virus, Cytomegalovirus, Herpes simplex virus might eventually lead to liver failure.
- Autoimmune hepatitis where the immune system attacks its own liver cells causing inflammation and injury.
- Metabolic diseases: Certain metabolic ailments can contribute to the development of liver failure. They are
Wilson’s disease (the liver is unable to filter out copper adequately and copper keeps building up in the liver, brain, eyes, and other organs) and acute fatty liver of pregnancy (that commonly occurs in the third trimester or soon after the delivery). - Drugs: Excessive consumption of Acetaminophen and certain prescription medications like Rifampicin and Isoniazid, Sodium valproate, Halothane, Zidovudine, and Didanosine can also cause liver failure.
- Toxins such as the poisonous wild mushroom Amanita phalloides.
- Vascular diseases like the Budd-Chiari syndrome can block veins of the liver.
- Liver cancer or other cancers that spread to the liver.
2. Chronic Liver Failure
The following conditions finally lead to scar tissue or cirrhosis that is the main cause of chronic liver failure.
- Liver disease that is caused due to heavy alcohol consumption for a decade or more.
- Fatty liver caused due to non-alcoholic reasons like obesity (40%), diabetes, protein malnutrition, coronary artery disease and consuming steroid medications.
- Chronic hepatitis C and B infections that cause inflammation and injury.
- Primary biliary cirrhosis where the bile dusts get damaged and primary sclerosing cholangitis which is a progressive liver disorder.
- Family history of overload of iron called hereditary hemochromatosis.
- Increased copper content in the liver called Wilson’s disease.
- Galactosemia - an uncommon hereditary condition which usually causes liver cirrhosis in infants is caused by increased levels of galactose, (which is a kind of sugar found in milk) in the blood because of deficiency of the liver enzyme required for its metabolic breakdown.
- Cystic fibrosis - a genetic disorder that affects the lungs.
- Autoimmune hepatitis.
- Drugs or toxins harmful to the liver.

What are the Symptoms and Signs of Liver Failure?
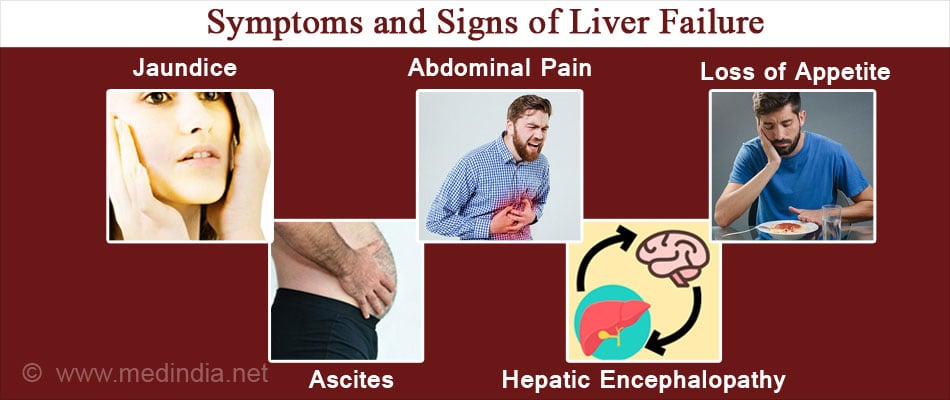
General symptoms and signs of acute liver failure are as follows:
- Weakness
- Nausea and vomiting
- Right upper abdominal pain
- Jaundice: manifests as yellowing of eyes, tongue, skin Liver might be enlarged initially, but it later shrinks and becomes difficult to palpate or feel by hand
- Accumulation of fluid in the abdominal cavity and edema develops later
- Hepatic encephalopathy characterized by change in brain function; it is caused due to a buildup of toxins in the bloodstream, which eventually cross the blood brain barrier and lead to brain damage. Symptoms could be reduced alertness, poor concentration, confusion and disorientation or as severe as coma
- Increased intracranial pressure
- Cerebral edema which is a prominent feature of liver failure
General symptoms and signs of chronic liver failure are as follows:
- Weakness
- Loss of weight
- Liver dysfunction due to the liver cells not working
- High blood pressure in the portal venous system - portal hypertension due to cirrhosis
- Ascites or protein-containing fluid that accumulates in the abdominal cavity, leading to abdominal swelling
- Increase in spleen size or splenomegaly
- Hepatic encephalopathy
- Acute kidney injury
What are the Complications of Liver Failure?
Complications are a very crucial part of liver failure, as they can increase the mortality rates in the patients. Complications might involve several organ systems, either in isolation or in combination.
- Neurological manifestations like cerebral edema, increased intracranial pressure (ICP) and encephalopathy.
- Sepsis occurs in fifty-five to eighty percent of the patients with liver failure. Bacterial infections are the commonest cause in seventy to eighty percent cases of sepsis and fungal infection occurs in about ten to twenty percent of these patients.
- Renal complications occur in thirty percent to seventy percent of patients with liver failure where drugs and toxins are the causative force behind liver failure and only three percent to five percent of patients where hepatitis viruses are the predominant cause of liver failure.
- Pulmonary complications: Lung infection is the commonest form of respiratory problem found in liver failure. In addition, acute respiratory distress syndrome, aspiration, and pulmonary edema may occur leading to respiratory failure.
- Cardiovascular complications and coagulopathy: Cardiac arrhythmia may set in due to electrolyte imbalance. Most proteins that promote or inhibit coagulation are synthesized in the liver. All coagulation factors are reduced in patients with liver failure. This may cause life-threatening bleeding, such as intracranial hemorrhage and gastrointestinal bleeding.
How do you Diagnose Liver Failure?
The development of hepatic encephalopathy, coagulopathy, and ascites is the indicator of development of liver failure, which can be seen by clinical signs. Various investigations used to diagnose and assess the severity of liver failure are:
- Urine examination shows the presence of protein, bilirubin and urobilinogen
- Blood examination shows increased number of white blood cells in the body which is an indicator of flare up of infections, and low blood platelet count which is responsible for excessive bleeding
- Blood serology is done to identify the presence of hepatitis causing viruses
- Liver function test shows increased serum bilirubin, increased serum aminotransferase activity and decreased levels of albumin in blood
- Prothrombin time is prolonged indicating higher tendency of bleeding and ineffective clot formation
- Elevated blood ammonia levels which get build up in the brain and lead to hepatic encephalopathy
- Electroencephalogram or EEG measures and records brain wave patterns; abnormalities show characteristics of hepatic encephalopathy
- Ultrasonography shows shrunken liver
- Intracranial pressure is raised
How do you Treat Liver Failure?
- All the patients diagnosed with liver failure should ideally be admitted to an intensive care unit. Simultaneously, the use of aggressive monitoring, and of respiratory support in the form of ventilator and oxygen administration and cardiovascular support should be provided to the patient especially if cerebral edema and hepatic encephalopathy have set in.
- If the patient gets into a coma, nutritional supplementation and feeding must be maintained by the feeding tube placed via the nose and inserted into the stomach.
- Transducers are placed inside the skull cavity to measure intracranial pressure and take remedial measures in case of rise of intracranial pressure.
- Prophylactic antibiotics and anti-fungal drugs are given by intravenous route. Dialysis is done if acute renal failure supervenes.
- The pathology behind hepatic encephalopathy is not completely understood but some association has been described between blood ammonia levels, intracranial hypertension, and the risk of brain hernia. Ammonia-lowering therapy with lactulose has been the mainstay of treatment for hepatic encephalopathy.
- Liver transplant: It is of two types:
- Orthotoptic liver transplant (OLT) - It is now the standard therapy for liver failure patients, who have a less than twenty percent chance of survival. Early transplant in such patients might reduce increased post-transplant mortality and morbidity. Contraindications to OLT are irreversible brain damage, uncontrolled bacterial infection in blood, human immunodeficiency virus infection, presence of any other malignant disease in addition to liver failure, and the presence of any other organ failure, which might hamper a satisfactory outcome of the transplant.
- Auxiliary liver transplantation (ALT) - It is another treatment option for liver failure patients. The native liver of patient is left inside the body even after transplant. This procedure aims to provide a temporary liver support until the original liver of the patient recovers. According to one study, the native liver regenerated in sixty-eight percent of those patients, who survived even after three months. After this, the donor liver can either be removed surgically or left in place to atrophy.
How do you Prevent Liver Failure?
Survival rate of patients with liver failure is approximately thirty-four percent. Two thirds of the deaths occur within the first seventy-two hours of hospitalization, which makes it clear that any therapeutic intervention for such patients must be started soon after hospitalization, and that early admission of such patients to advanced tertiary care centers must be promoted. The median survival time is 4 days. Viral hepatitis must be immediately treated with antiviral drugs and the condition must not be allowed to complicate and develop into liver failure.