- Dermnetnz-Kwashiorkor-Author: Vanessa Ngan - (https://www.dermnetnz.org/topics/kwashiorkor/)
- INCAP studies of kwashiorkor and marasmus- Nevin S. Scrimshaw and Fernando E. Viteri - (https://pdfs.semanticscholar.org/0f14/7fb539e150ed977e3f6425edd0d97aeb3719.pdf )
- Epidemiology and Prevention of Severe Protein Malnutrition (Kwashiorkor) in Central America - NEVIN S. SCRIMSHAW, Ph.D., M.D., F.A.P.H.A.; MOISCS BEHAR, M.D.; FERNANDO VITERI, M.D.; GUILLERMO ARROYAVE, Ph.D.; and CARLOS TEJADA, M.D. - (https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.47.1.53)
- Mother and child nutrition- Management of Malnutrition in Children Under Five Years - (http://motherchildnutrition.org/malnutrition- management/info/medical-complications.html)
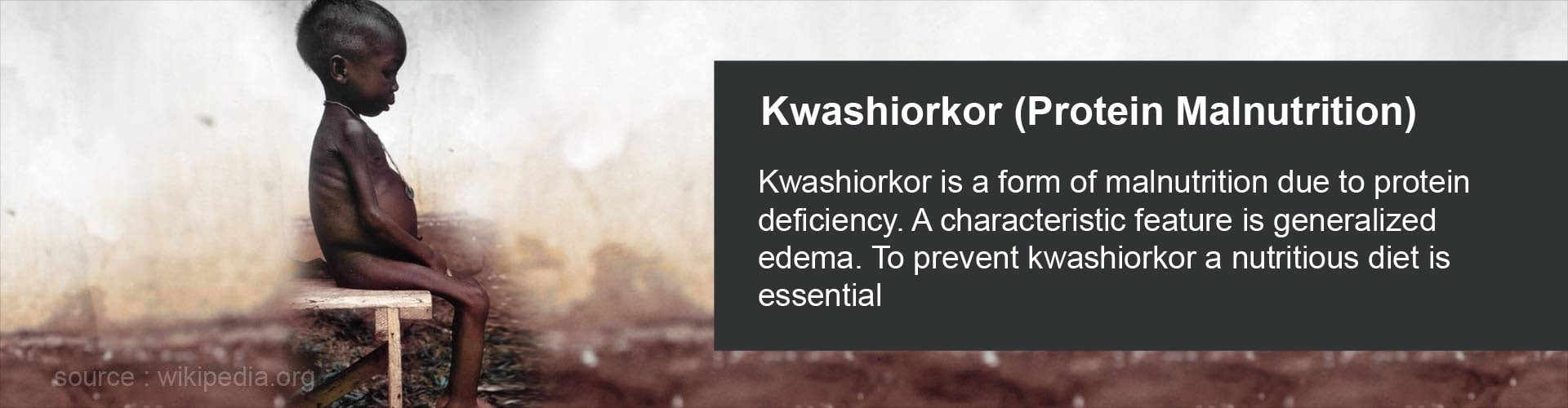
What is Kwashiorkor?
Kwashiorkor is a severe form of malnutrition caused by the lack of proteins in the diet. Kwashiorkor is a type of protein energy malnutrition (PEM) which is widespread in infants and children throughout the developing world
.Marasmus is another form of protein energy malnutrition where there is deficient intake of both calories and proteins due to starvation whereas kwashiorkor is due to severe lack of protein in the diet with adequate energy intake.
Kwashiorkor usually affects infants and children, most often around the age of weaning up to five years of age. Kwashiorkor is also known as "edematous malnutrition" as it always includes edema, especially of ankles, feet, face and belly
.Kwashiorkor is also known as protein calorie malnutrition, protein energy malnutrition and malignant malnutrition.
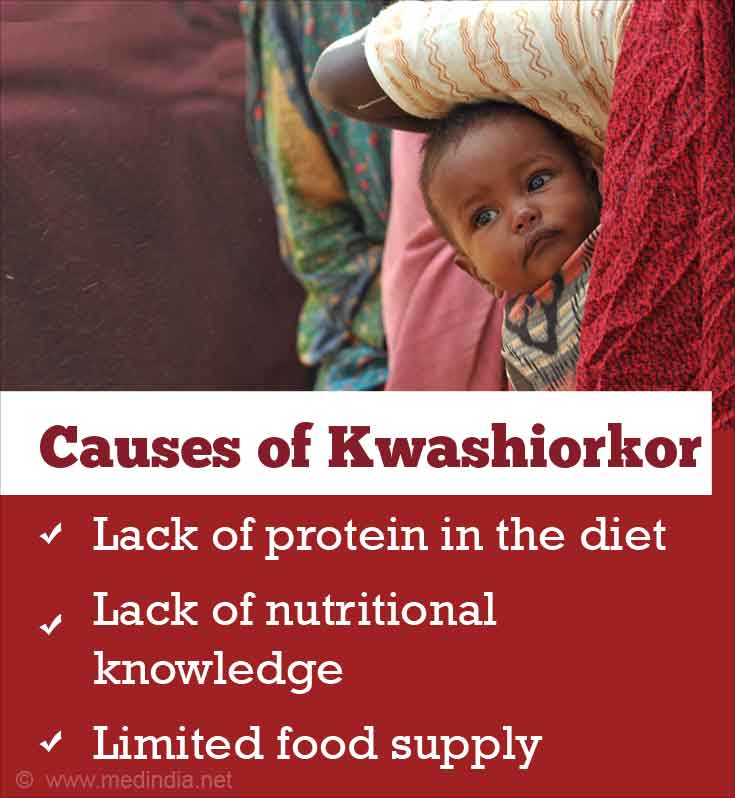
What are the Causes of Kwashiorkor?
The main cause of kwashiorkor is a lack of protein in the diet. The reasons include
- Lack of nutritional knowledge,
- Limited food supply eg sub Saharan Africa, Central America and Southeast Asia
- Regional dependence on low protein diets, such the maize based diets can also cause children to develop this condition.
- Serious infections such as septicemia, pneumonia, gastroenteritis, tuberculosis, measles and AIDS often precipitate kwashiorkor.
- In developed countries kwashiorkor is rare and is a result of long term illness, regular intake of junk food, fad diets or due to an underlying condition, such as HIV.
What are the Symptoms and Signs of Kwashiorkor?
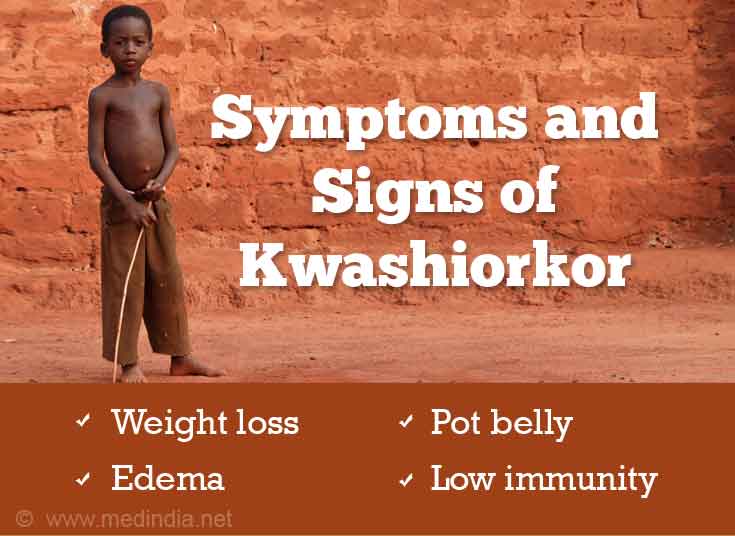
- Early signs of kwashiorkor resemble general symptoms of malnutrition such as lethargy, fatigue and irritability.
- If, however protein deprivation continues there is failure to put on weight and gain height, along with loss of muscle mass
- Presence of generalized swelling (edema) and a large protuberant pot belly due to fluid accumulation. There is edema of the legs and the face looks plump and swollen.
- The child’s weight is usually below sixty to eighty percent of standard weight but some infants may have a normal weight because of their edema.
- There is enlargement of liver due to anemia.
- There may be frequent episodes of illness such as diarrhea due to low resistance power and a delay in recovery from illnesses.
- They often have signs of anemia such as pale skin and nails and enlargement of the liver.
- Due to vitamin deficiencies symptoms such as sparse, thin, reddish hair, soreness and painful cracking of mouth, increased or decreased skin pigmentation with scaling are common.
- Protein deficiency leads to a failing immune system which makes the children prone to infections and the normally mild infections are more severe and take a longer recovery period.
How do you Diagnose Kwashiorkor?
- Kwashiorkor is mostly diagnosed based on a child's physical appearance, clinical and dietary history.
- Other tests include growth measurements, body mass index (BMI) and complete physical examination.
- Physical examination may show an enlarged liver and generalized swelling (edema).
- Laboratory tests may show anemia, low blood sugar and total serum protein, iron, potassium, magnesium, urea and increased levels of growth hormone.
- Hair analysis or skin biopsy may also be performed in some cases.
How do you Treat Kwashiorkor?
- Kwashiorkor treatment starts with correcting fluid and electrolyte imbalances.
- Your doctor will also recommend vitamin and mineral supplements.
- If kwashiorkor is identified early it can be treated with either specially formulated milk based feeds or ready to use therapeutic food (RUTF) which is typically made up of peanut butter, milk powder, sugar, vegetable oil, and added vitamins and minerals.
- Any infections should also be treated appropriately.
- Once the condition is stabilized, small amounts of food should be introduced gradually.
- Food must be reintroduced slowly, carbohydrates first to provide energy, followed by protein foods.
- More intensive treatment in hospital will be needed in severe cases or where there are complications, such as infections.
- Treatment given early in the course of the disease generally produces a good recovery.
What are the Complications of Kwashiorkor?
- Children with kwashiorkor may have permanent physical and mental disabilities. The children may not reach their full growth and height potential.
- There may be muscle wasting, hepatomegaly, hypoprotenemia, hyper pigmentation and a lowered immunity.
- Electrolyte imbalances, especially potassium deficiency and iron deficiency may occur. These may lead to bleeding, malabsorption, tremors and heart failure.
- There may be hypothermia and hypoglycemia due to loss of energy stores.
- Kwashiorkor can be fatal if it's left untreated for too long because children become very vulnerable to infections.
- If left untreated kwashiorkor can lead to coma, shock, or death.
How do you Prevent and Manage Kwashiorkor?
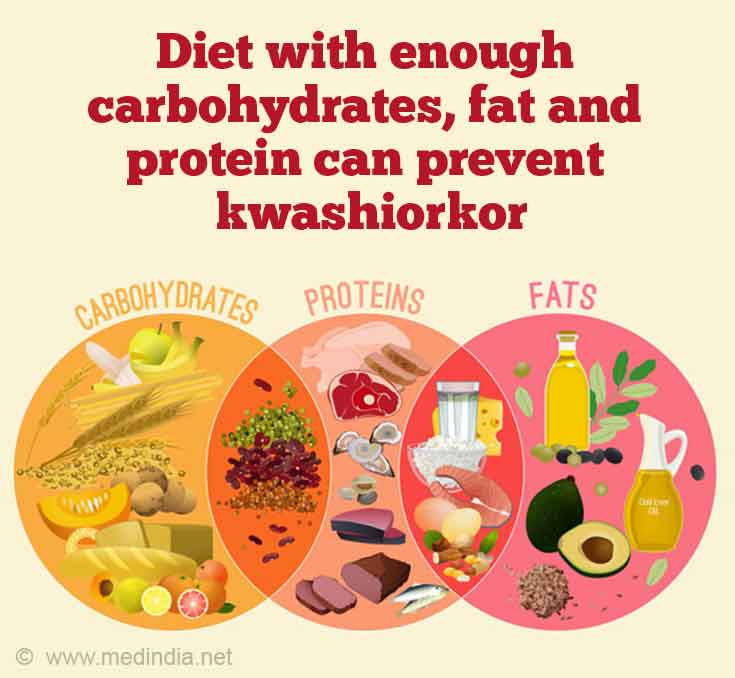
- To prevent kwashiorkor, children should be given nutritious food.
- The diet should have enough carbohydrates, fat (at least ten percent of total calories), and protein (twelve percent of total calories).
- Mineral and vitamin supplements along with formulated milk based feeds are essential, especially in areas where there is continuous scarcity of food due to famine or droughts.
- There should be promotion of proper food fortification practices.
- Proper education and awareness about breast feeding and weaning practices can go a long way in preventing nutritional diseases such as kwashiorkor.
- There should be a provision of immunization for all children in poor countries.
- Pregnant and lactating women should be given sufficient amount of nutritious food and;
- Women should be encouraged to breast feed their infants.