- Karl Landsteiner and the first human marker locus - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc1461144/)
- Fetal middle cerebral arterial Doppler assessment - (https://radiopaedia.org/articles/fetal-middle-cerebral-arterial-doppler-assessment)
- Blood groups systems - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4260296/)
- Rh disease (Erythroblastosis fetalis) - (https://www.cedars-sinai.edu/patients/health-conditions/rh-disease-erythroblastosis-fetalis.aspx)
What is Erythroblastosis Fetalis?
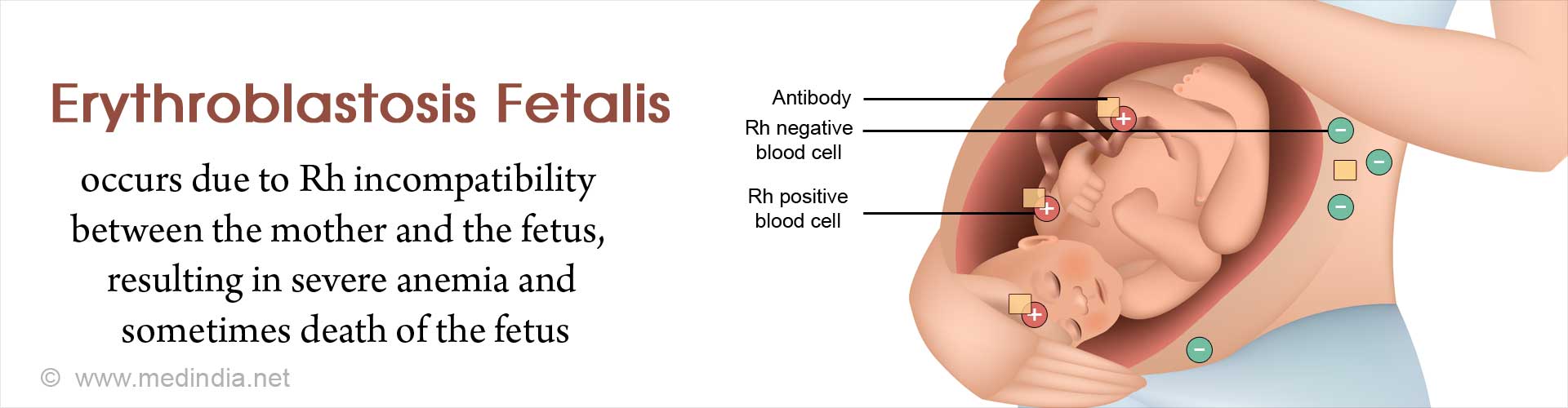
Erythroblastosis fetalis, also called hemolytic disease of the newborn (HDN), usually occurs in the fetus, but can also occur in the neonate (erythroblastosis neonatorum). It is a type of anemia in which the red blood cells (RBC) of the fetus are destroyed by maternal antibodies in an immune response targeted against the fetus. This occurs due to incompatibility of the blood groups of the mother and fetus, which arises when the fetus inherits a certain blood group factor from the father that is absent in the mother. As a result, the baby can suffer from severe anemia, brain damage, or even death.
What are the Causes of Erythroblastosis Fetalis?
Erythroblastosis fetalis can be caused due to incompatibility of either of two major blood types. These include Rh incompatibility and ABO incompatibility.
Hemolytic Disease of the Newborn – An Example of Rh Incompatibility
The Rh system of blood grouping is based on the presence or absence of the Rh factor on the surface of RBC. This factor is an inherited protein antigen that was first discovered in rhesus monkeys, hence called “Rh” based on the first two letters of the word “rhesus”. Not all people have the Rh factor. Those who have this factor are said to be Rh-positive (Rh+) or D-antigen positive and those who do not, are said to be Rh-negative (Rh¯).
- An Rh¯ mother can conceive an Rh+ fetus, if the father is Rh+.
- During delivery, the fetal RBC may enter the maternal circulation due to leakage.
- As a result, the immune system of the mother generates antibodies against the fetal Rh factor-bearing RBCs.
- The first born is usually spared since the maternal antibodies are formed only after delivery.
- If the mother again becomes pregnant with an Rh+ fetus, her antibodies can cross the placenta and attack the fetal RBCs, thereby causing severe hemolytic anemia.
- The fetal bone marrow reacts to the hemolytic anemia by releasing immature RBCs called erythroblasts into the fetal peripheral circulation, causing erythroblastosis fetalis.
ABO Incompatibility
The ABO system is another system of blood grouping discovered by Karl Landsteiner, for which he received the Nobel Prize in Physiology or Medicine for the year 1930. This system is based on the presence or absence of the A and B protein antigens on the surface of RBC. When only the A antigen is present, the blood group is A. When only the B antigen is present, the blood group is B. When both A and B antigens are present, the blood group is AB. If both A or B are absent, the blood group is O. ABO incompatibility disease is almost exclusively limited to fetuses with A or B antigens whose mothers have blood group O. Approximately one-third of fetuses have the mother’s antibodies in their circulation, but only a small percentage develop symptoms of ABO incompatibility disease. ABO incompatibility is considered to be less harmful to the fetus than Rh incompatibility.
Incompatibility arising from Minor Blood Groups
There are other minor blood group antigens that the fetus may carry, which can increase the risk of erythroblastosis fetalis. These blood groups include Kell, Duffy, Kidd, Lutheran, Diego, Xg, P, Ee, Cc and MNS.
What are the Symptoms and Signs of Erythroblastosis Fetalis?
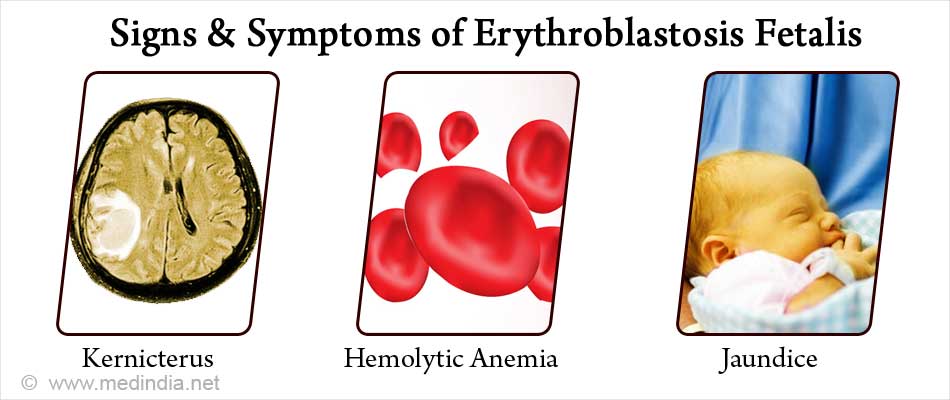
The clinical features of erythroblastosis fetalis result from destruction of fetal RBCs by maternal antibodies against them. They can range from mild anemia and jaundice to fetal death in utero.
The major symptoms of erythroblastosis fetalis are briefly discussed below:
- Jaundice: This occurs due to the deposition of bilirubin (breakdown product of hemoglobin from RBC) in the skin and the whites of the eyes. This imparts a yellowish color to these structures.
- Hemolytic Anemia: This occurs due to the destruction of RBCs. Untreated anemia can cause heart failure, enlarged liver and/or spleen, generalized swelling and respiratory distress.
- Kernicterus: This occurs due to the deposition of bilirubin in the brain and spinal cord. This can lead to nerve cell degeneration, hearing loss, mental retardation, and even death.
- Hydrops Fetalis: This is the severest form of the disease in newborns and is characterized by extreme edema (abnormal accumulation of serous fluid) in unusual places like the abdominal cavity, heart and lungs. This can lead to congestive heart failure as the extra fluid causes increased pressure on the heart, reducing its pumping ability. Moreover, fluid accumulation in the lungs prevents normal breathing, because the lungs cannot expand fully.
How do you Diagnose Erythroblastosis Fetalis?
Blood Tests
- Indirect Coombs test is done on the mother’s blood if she is found to be Rh-, during the antenatal visit and the father is Rh+. It measures the number of antibodies in the maternal blood. If the Rh¯ mother does not have antibodies during initial testing, then she will be tested again at 18 to 20 weeks of pregnancy and again at 26 to 27 weeks. If anti-Rh antibodies are detected at any of these time-points, then treatment is initiated.
- Direct Coombs test is carried out on the fetal blood sample which measures the level of maternal antibodies attached to the baby’s RBCs. This test is done if the fetus shows features of anemia and jaundice.
- Tests to determine fetal blood counts to check for anemia and serum bilirubin levels to check for jaundice.
In another scenario, the baby may develop jaundice after birth, in spite of the fact that there is no Rh incompatibility. Under these circumstances, the symptoms can be attributed to ABO incompatibility. However, the symptoms are much milder than in case of Rh incompatibility.
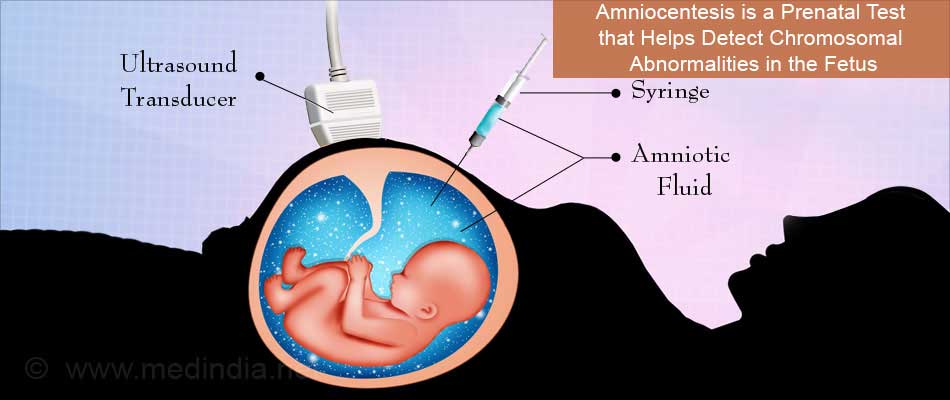
The doctor may recommend a non-invasive test to detect fetal middle cerebral artery blood flow by means of Doppler ultrasound. If the baby’s blood flow is affected, then erythroblastosis fetalis is suspected.
This procedure is used to sample the amniotic fluid that surrounds the developing fetus inside the uterus. A needle is inserted into the amnion (the sack filled with amniotic fluid) using ultrasound guidance to take a fluid sample. This is tested in the lab to assess the baby’s risk of anemia. Moreover, analysis of the amniotic fluid can measure the bilirubin concentration to predict the severity of the disease. If the levels are elevated, then intrauterine transfusion with Rh¯ blood can be given until premature delivery can be induced.
How do you Treat Erythroblastosis Fetalis?
Before the baby is born, the following treatment strategies may be adopted:
- Blood Transfusion: The baby may require blood transfusions before birth in order to treat anemia. Intrauterine blood transfusion is given through the umbilical cord.
- Pre-term Delivery: In certain situations, the baby needs to be born before its full-term. Therefore, when the baby’s lungs and heart mature enough for delivery, the doctor may advise delivering the baby pre-term (usually between 32 to 35 weeks).
After birth, the baby may need to be given further blood transfusions. Fluids may be administered intravenously to increase low blood pressure. Mechanical respiratory support may need to be provided to treat respiratory insufficiency. Some specific strategies that may be adopted are briefly highlighted below:
- Exchange Transfusion: This is a special type of transfusion in which the baby’s blood is exchanged with that of the donor’s blood. In this procedure, the anti-Rh antibodies (produced by the mother’s incompatible blood) that are destroying the baby’s RBC are removed, along with excess bilirubin. Small samples of the baby’s blood are taken out and simultaneously replaced with the donor’s blood. This procedure may have to be repeated several times.
- Phototherapy: This is also called light therapy and is used to treat jaundice. The light treatment helps to convert the bilirubin in the baby’s skin to a form that can be excreted by the baby. The baby is usually placed on its back and illuminated from above by a special light. Nowadays, flexible light pads are also available that wrap around the baby. The eyes are kept covered to protect from contact with the light.
- Immunoglobulin: Intravenous immunoglobulin (IVIG) to neutralize maternal anti-D antibodies. These can be administered with the aim of reducing RBC breakdown and lowering the levels of circulating bilirubin. IVIG can be used to reduce the need for exchange transfusion and to shorten the length of phototherapy.
How do you Prevent Erythroblastosis Fetalis?
Erythroblastosis fetalis can be prevented by carrying out screening tests and by the administration of Rh factor immunoglobulins to the pregnant mother. These aspects are briefly discussed below:
- Screening: The pregnant mother’s blood type should be tested at the first prenatal visit. Besides testing for Rh type, other blood types may also be tested. In case of previous pregnancies or a history of blood transfusions, further tests may be required. The father’s blood may also be tested for ABO and Rh types. During pregnancy, the baby’s blood may also need to be tested for ABO and Rh types and as well as to see if it reacts with the maternal blood.
- Rh Factor Immunoglobulins: If the pregnant mother is at risk of Rh sensitization, it is recommended that Rho (D) immunoglobulin (RhoGAM) be administered at 28 weeks of gestation and within 72 hours of delivery. This medicine contains high titers of anti-Rh antibodies, which neutralize Rh+ fetal RBCs. Because fetal-maternal transfer and likelihood of sensitization is greatest at termination of pregnancy, the preparation is given within 72 hours after delivery or termination of pregnancy due to miscarriage, abortion, or ectopic pregnancy. The standard dose is 300 µg of RhoGAM by the intramuscular (IM) route. A rosette test can be used to rule out significant fetal-maternal hemorrhage (FMH). However, it should be noted that there is no comparable immunotherapy available for other blood group incompatibilities.
Health Tips:
- Talk to your doctor regarding antibody screens: If you are pregnant you should be screened for blood type, Rh type, anti-Rho (D) and other antibodies that may cause erythroblastosis fetalis.
- Deliver your baby at a hospital equipped to handle pregnancy-related emergencies: If blood tests have confirmed that your baby may have erythroblastosis fetalis, it would be wise to have the delivery in a hospital having all facilities and trained personnel to handle an emergency.
- Consult your gynecologist if you are pregnant and experiencing vaginal bleeding: You should immediately consult your gynecologist if you experience vaginal bleeding at any time during your pregnancy. Prompt treatment will prevent further complications at later stages of pregnancy.
- Keep an eye on your newborn baby’s health: Check for the following: (i) fever; (ii) jaundice (yellowing of skin); (iii) feeding less than normal; (iv) passing less urine than normal.