How do you Diagnose Neutropenic Sepsis?
The diagnosis of neutropenic sepsis requires careful consideration of the symptoms to ensure the right treatment is provided. In certain cases, if cancer patients undergoing treatment do not show fever, they may not be suspected with neutropenic sepsis.
Hence, it is important to maintain a level of caution by examining even those cancer individuals undergoing treatment, who may be unwell in the absence of fever. This can especially happen in those who take steroids and so inflammation is diminished during chemotherapy. As a result, the usual symptoms of fever are not observed.
- A full diagnostic examination should involve a complete medical examination and physical history.
- Following this, the chest should be examined for circulation and breathing issues. The oropharynx, the internal regions (e.g. cardiac, brain, bones), and the skin must be checked for potential bacterial infections.
- Samples from urine, from lesions on the skin, or from diarrhea should be examined for infection.
- A digital rectal examination could cause potential infection to develop in the gut and is not generally advised.
- In addition, the neutrophil count in the blood, blood culture, the level of C-reactive protein, and the levels of kidney and liver proteins should be assessed for sites of infection.
- Elevated serum lactate levels and reduced serum bicarbonate levels are good indicators of a neutropenic sepsis infection.
- Similarly, elevated C-reactive protein indicates a poor outcome of the infection. These indicators are useful in determining the antibiotic course.
How do you Treat Neutropenic Sepsis?
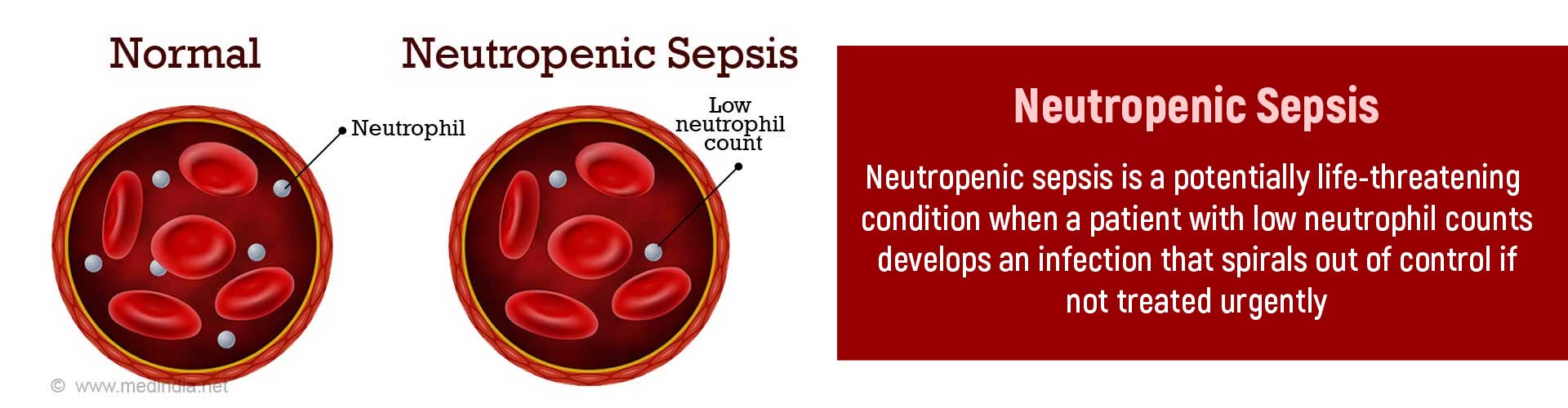
The recommendation to begin treatment for neutropenic sepsis is based on a falling neutrophil count that is less than 0.5 x 109/litre and the presence of fever or temperatures that are higher than 38°C or lower than 36°C.
The first step is to intravenously treat the patient with broad spectrum antibiotics and crystalloid fluids within the first hour of detection. It should be noted that if treatment is delayed till the confirmation of neutropenia, then the individual is likely to die. Antibiotic monotherapy with piperacillin and tazobactam is recommended. Aminoglycoside therapy (e.g. gentamycin) with antibiotics is not generally favored.

Following the treatment, the patient’s blood should be obtained from a central blood vessel as well as from peripheral sources. The blood samples can then be investigated for infection. Similarly, a chest x-ray and analysis of the urine sample (in children) are additional ways to confirm bacterial infection.
However, it has been noted that those individuals whose sepsis is resolved may still be susceptible to death in the ICU due to the failure of multiple organs, such as hepatic, respiratory, renal, or circulatory. Sometimes, they contract a secondary bacterial infection due to the organ failure.
The patient should be monitored for the next 48 hours after beginning antibiotic treatment. In patients who do not show any complications, they should be monitored daily and the presence of any potential existing risk factors should be investigated. If fever persists following 48 hours, it means there is some other type of infection e.g. a fungal infection. If the fever continues beyond 5 days, then the patient should be checked with a chest CT scan. Experts in clinical microbiology and infectious diseases should be consulted and, if needed, antifungal medications (e.g. liposomal amphotericin B, caspofungin, voriconazole) should be initiated.
If there is no fever following 48 hours, then the intravenous infusion of antibiotics may be switched to oral antibiotics. Eventually after a week, the antibiotics may be discontinued. The neutrophil count may not be more than 0.5 x 109/l at this point.
Patients with neutropenia can be given Granulocyte-colony stimulating factor (G-CSF) injections to stimulate the marrow to produce granulocytes to help fight recurrent infections. The most commonly used agent is filgrastim.
How can you Prevent Neutropenic Sepsis?
Taking the following precautions may help prevent or reduce risk of neutropenic sepsis in a patient with neutropenia
- Maintain good personal hygiene and frequent handwashing
- Avoid crowds and persons who are unwell
- Using soft toothbrush
- Washing and cooking food thoroughly before eating
- Regular bathing and shower
- Wear footwear when going outdoors
- Being careful while shaving