- Blue Skin or Lips (Cyanosis) - National Health Service (NHS), UK - (https://www.nhs.uk/conditions/blue-skin-or-lips-cyanosis/)
- Blue Discoloration of the Skin - Medline Plus: U.S. National Library of Medicine - (https://medlineplus.gov/ency/article/003215.htm)
What is Cyanosis?
Cyanosis is the discoloration of the skin or mucus membranes, assuming a bluish or purplish tinge due to the decreased supply of oxygen (hypoxia) to the underlying tissues. The term “cyanosis” is derived from the Greek word kuaneos meaning “dark blue”.
Oxygen Transport by Blood in the Body
Oxygen in blood is carried primarily by the globulin metalloprotein hemoglobin, as oxyhemoglobin in the arteries, which is bright red in color. It releases the oxygen to the various tissues and becomes deoxygenated in the process (deoxyhemoglobin). This blood is bluish or purplish in color, giving the skin and mucous membranes their characteristic tinge. Cyanosis is said to occur when the level of deoxyhemoglobin in blood becomes higher than 5g/dl.
What are the Different Types of Cyanosis?
Cyanosis is of two types – central and peripheral. The characteristic features of these two types of cyanosis include the following:
Central Cyanosis
This condition occurs due to heart and lung conditions, as well as the occurrence of abnormal forms of hemoglobin, such as methemoglobin and sulfhemoglobin in the blood. These are responsible for the blue-purple discoloration of the tongue and the lining of the oral cavity. It has been observed that central cyanosis can be accompanied by peripheral cyanosis. However, in the absence of peripheral cyanosis, the toes and fingers usually exhibit a warm sensation to touch.
Peripheral Cyanosis
This occurs due to the decreased blood flow to the peripheral parts (extremities) of the body, such as the fingers, toes and especially the nail beds. Peripheral cyanosis is accentuated by the stagnation of arterial blood in the capillaries of the periphery and release of most of the oxygen to the tissues. As a result, the level of deoxygenated blood increases in the capillaries and veins. This can occur due to congestive heart failure and shock, both of which exhibit sluggish blood circulation and rapid fall in blood pressure in the capillaries and veins. Peripheral cyanosis is also precipitated by exposure to extremely cold temperatures such as higher altitudes, as well as vascular diseases. Peripheral cyanosis responds well to warming-up the limbs.
What are the Causes of Cyanosis?
The causes of cyanosis vary with the type i.e. central or peripheral. Central cyanosis is further subdivided into (i) central cyanosis in newborns and (ii) central cyanosis in adults.

Central Cyanosis in Newborns: The causes of central cyanosis in newborns include cardiac and respiratory conditions.
Some cardiac complications (due to low oxygen content of the blood) responsible for central cyanosis in newborns include the following:
- Transposition of the great arteries
- Fallot’s tetralogy
- Atrial septal defect
- Stenosis / atresia of the pulmonary or tricuspid valve
- Truncus arteriosus
- Hypoplastic left heart
- Persistent fetal circulation
Some respiratory complications (inability to oxygenate blood) responsible for cyanosis in newborns include the following:
- Respiratory distress syndrome
- Birth injury / birth asphyxia
- Pneumothorax
- Pleural effusion
- Pulmonary edema
- Obstruction of the upper respiratory tract
Central Cyanosis in Adults: Adult central cyanosis can be caused by several conditions. Some of these are briefly highlighted below:
- Pulmonary embolism
- Pulmonary edema
- Severe pneumonia
- Chronic obstructive pulmonary disease
- Acute adult respiratory distress syndrome
- Acute severe asthma
Peripheral Cyanosis Peripheral cyanosis manifests as a bluish discoloration of the hands and feet. The underlying reason is inadequate delivery of oxygenated blood to the tissues of the hands and feet. The causes of inadequate supply of oxygenated blood include the following:
- All causes of central cyanosis
- Tight clothing or jewellery cutting off blood flow
- Deep vein thrombosis (DVT)
- Heart failure
- Arterial / venous insufficiency
- Raynaud’s syndrome (pain and bluish discoloration of extremities on cold exposure)
- Low blood pressure (hypotension)
- Beta-blockers
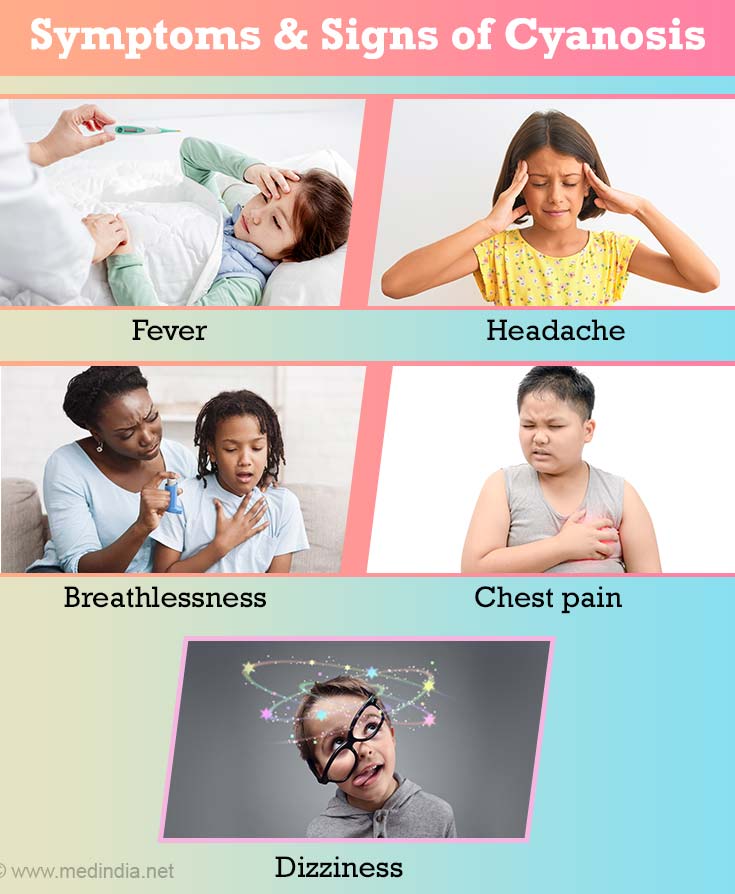
What are the Symptoms and Signs of Cyanosis?
The cardinal clinical feature of cyanosis is a bluish purple discoloration of the skin and perioral area, such as the tongue, lips and inner lining of the mouth (central cyanosis) or in the extremities such as the tips of the fingers and toes, nail beds, hands, and feet (peripheral cyanosis). If this clinical symptom is accompanied by the following symptoms and signs, it could indicate a medical emergency:
- Fever
- Headache
- Breathlessness / difficulty breathing / rapid shallow breathing
- Chest pain
- Dizziness / fainting
- Profuse sweating
- Raynaud’s phenomenon
- Cold fingers and toes
How do you Diagnose Cyanosis?
Besides the obvious clinical signs such as the blue or purplish tinge on the skin, there are certain other definitive diagnostic tests for confirming and consolidating the clinical findings. These include the following:
Auscultation: This method involves examination of the chest (lungs and heart) by using a stethoscope. This will indicate whether there are any problems in these organs that could result in cyanosis.
Chest X-Ray: A chest X-ray can detect any lung abnormalities that could support the clinical findings.
Electrocardiography: An electrocardiogram (ECG) is used to detect any heart abnormalities, based upon the clinical findings.
Complete Blood Count (CBC): CBC helps to determine the level of hemoglobin in the blood and detect if anemia is present.
Pulse Oximetry: This is a non-invasive method in which a clip-like device is attached to the finger, which indirectly records the oxygen saturation of the blood and changes in blood volume in the skin. The device works by illuminating the skin and measures changes in light absorption. The readings are displayed on a portable monitor, which is technically termed as a photoplethysmogram.
Arterial Blood-Gas Analysis: It is also known as the arterial blood-gas (ABG) test. This is an invasive blood test in which a small amount of blood is drawn from an artery and the concentrations of oxygen and carbon dioxide, as well as the pH of arterial blood are measured. The ABG test provides an insight on how efficiently the red blood cells (RBC) are able to transport oxygen and carbon dioxide in the body.
How do you Treat Cyanosis?
There are several strategies for treating cyanosis. Some of these provide symptomatic relief, while others treat the underlying condition. These are briefly highlighted below:
Heat Therapy: Application of mild heat to the affected areas can dramatically improve the symptoms of peripheral cyanosis.
Oxygen Therapy: Oxygenation is crucial for stabilizing a hypoxic patient and is often used in conjunction with a ventilator that provides artificial respiration. Oxygen therapy brings about a rapid improvement of the condition.
Intravenous Fluids: Fluids containing nutrients may need to be administered intravenously to babies who have difficulty in feeding orally due to cyanosis caused by an underlying heart disease. Glucose infusions may be given in case of low blood glucose levels.
Drug Therapy: Drugs are required for treatment of many of the underlying conditions. Some examples are given below:
- Diuretics are administered to heart failure patients presenting with excessive accumulation of fluids in the body.
- Drugs are used to improve the pumping efficiency of the heart, as well as to treat any abnormalities in the heartbeat and heart rhythms.
- Antibiotics are prescribed for treatment of respiratory infections like pneumonia.
- Babies suffering from transposition of great arteries (TGA) or tricuspid atresia require the administration of prostaglandins after birth.
- Patients suffering from patent ductus arteriosus can be treated with indomethacin or ibuprofen.
Surgery: Surgical intervention is required for treatment of congenital heart defects such as Fallot’s tetralogy. In this condition, open heart surgery is required soon after birth in order to surgically correct the defects. In case of congenital defects that are less severe, the surgery can usually wait till the baby reaches 3 to 6 months of age.