- The Complex Pathogenesis of Bacteremia - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3916384/)
- Red Blood Cell Distribution Width is an Independent Predictor of Mortality in Patients with Gram-negative Bacteremia. - (https://www.ncbi.nlm.nih.gov/pubmed/22683729)
- Age-related Differences in Symptoms, Diagnosis and Prognosis of Bacteremia. - (https://www.ncbi.nlm.nih.gov/pubmed/23883345)
- The Clinical Importance of Microbiological Findings in the Diagnosis and Management of Bloodstream Infections. - (https://www.ncbi.nlm.nih.gov/pubmed/19374579)
- Staphylococcus Aureus Bloodstream Infections: Definitions and Treatment. - (https://www.ncbi.nlm.nih.gov/pubmed/19374581)
- Bloodstream and Intravascular Catheter Infections - (https://www.ncbi.nlm.nih.gov/books/nbk7008/)
- Duration of Antibiotic Therapy for Bacteremia: A Systematic Review and Meta-Analysis. - (https://www.ncbi.nlm.nih.gov/pubmed/22085732)
- Staphylococcus Aureus Bacteremia: Epidemiology, Pathophysiology, and Management Strategies. - (https://www.ncbi.nlm.nih.gov/pubmed/19374578)
What is Bacteremia?
As the name suggests, bacteremia is a condition where viable bacteria are present in the bloodstream of an individual.
Bacteremia can result either from surgical procedures, such as dental surgeries, or activities like brushing teeth, or due to infections.(1✔ ✔Trusted Source
The Complex Pathogenesis of Bacteremia
Go to source)

In most cases, the body’s immune system deals with these bacteria and removes them from the blood. However, when the body’s defense mechanism fails or if there is a foreign substance present, or a lesion, the bacteria in the blood multiply, leading to sepsis or life-threatening infection.
The clinical outcome of bacteremia is affected by factors, such as:
- Treatment with antibiotics
- Other co-morbidities such as diabetes
- Surrounding environment, and
- Age and health status of individuals.
Bacteremia might be either acquired in the hospital or community-related. The most common sites for bacterial infection are the urinary tract, skin, oral cavity, gastrointestinal tract, and respiratory tract.
Bacteremia may be categorized as transient, intermittent, and persistent based on the duration of symptoms.
- Transient bacteremia: This infection is present for a brief period of time (few minutes to a few hours), such as following a gastrointestinal biopsy, surgical drainage, or dental operations. Harmless transient infections are those that occur when defecating, brushing our teeth, intravenous injection of drugs, or abrasions on the skin surface due to injuries.
- Intermittent bacteremia: This type of infection is seen at intermittent periods as the same microorganism affects the individual. Such infections are observed in connection with abscesses and infections, such as osteomyelitis, pneumonia, and spondylodiscitis.
- Persistent bacteremia: Intravascular infections (e.g. thrombus infection, aneurysm), infective endocarditis (heart valve infections), and systemic bacterial infections (e.g. typhoid) are examples of persistent bacteremia.
Bacteremia can also be classified as primary or secondary depending on whether the blood infection occurred directly or spread from another site.
- Primary bacteremia is caused by direct contact with an infected needle that releases drugs directly into the bloodstream or due to an infected internal catheter in the body.
- Secondary bacteremia occurs secondary to infection in other sites (e.g. skin and soft tissues), pneumonia, and infection in wounds. The bacteria leave the infection site and enter the bloodstream.(2✔ ✔Trusted Source
Bloodstream and Intravascular Catheter Infections
Go to source)
What are the Causes of Bacteremia?
Based on an analysis of bacteremia cases, it has been observed that bacteremia is a result of numerous microorganisms that invade the body. The effectiveness of the body’s immune system determines the severity of the bacteremia infection. At the same time, the variations in disease intensity are due to genetic differences in individuals.
The physical location, age and health of the individual, the surrounding environment, and the type of bacteria involved, influence how bacteremia is caused.
Hospital acquired bacteremia
The causes of hospital bacterial infections (nosocomial infections) are easy to guess. They include:
- Intravenous drug delivery
- Surgery
- Invasive or internal device used (e.g. implanted devices, catheters)
- Infected skin ulcers
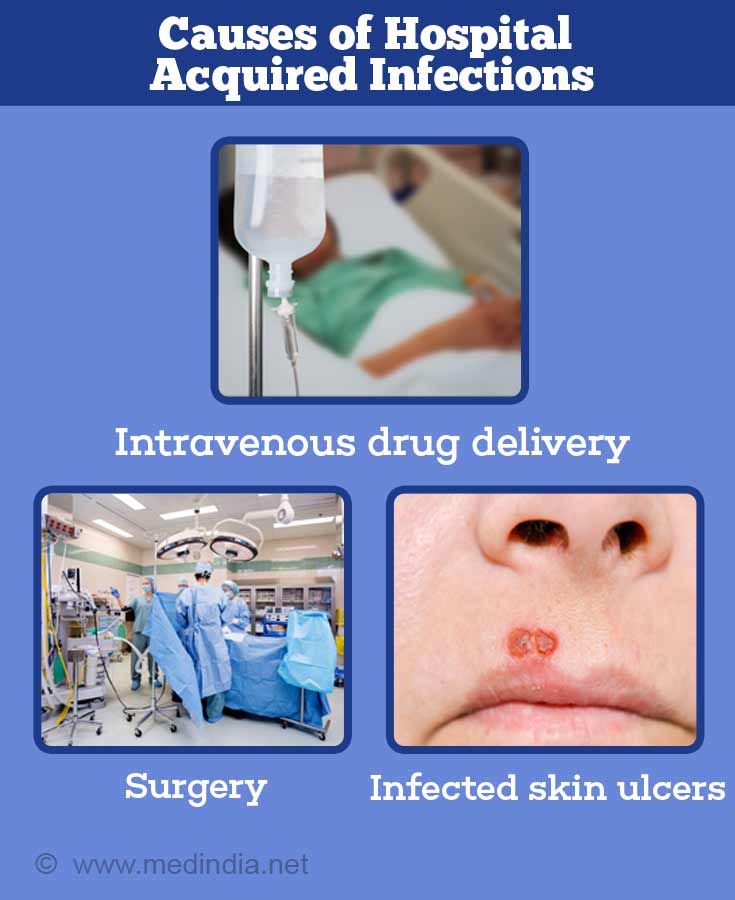
Hospital (nosocomial) infections are mainly caused by Gram-positive bacteria (e.g. Enterococci, Streptococci, Staphylococcus aureus, Staphylococcus epidermis, Clostridia).
Staphylococcus aureus is the most common bacteria involved in hospital infections in Latin and North America. In Europe, S. aureus is responsible for the second largest majority of hospital infections.
Community Acquired Bacteremia
Gram negative bacteria are more commonly implicated in community acquired bacteremia. Staphylococcus is also an important cause.
Gram-negative bacteria (e.g. Pseudomonas aeruginosa, Klebsiella pneumoniae, Enterobacter aerogenes, Escherichia coli) are responsible for 30% of the bacteremia cases. Gram-negative bacteremia occurs most often due to infections reaching the bloodstream from respiratory tract, gastrointestinal tract, genitourinary tract and liver and biliary tract infections. It is seen more commonly in elderly (older than 65 years) and is associated with an increased death and morbidity.(3✔ ✔Trusted Source
Red Blood Cell Distribution Width is an Independent Predictor of Mortality in Patients with Gram-negative Bacteremia.
Go to source)
The risk factors for developing bacteremia include:
- Underlying diabetes with uncontrolled blood sugar levels
- HIV infection which suppresses the immune response
- Treatment with immunosuppressants following transplant surgery
- Liver disease
- Long-term hemodialysis for kidney disease
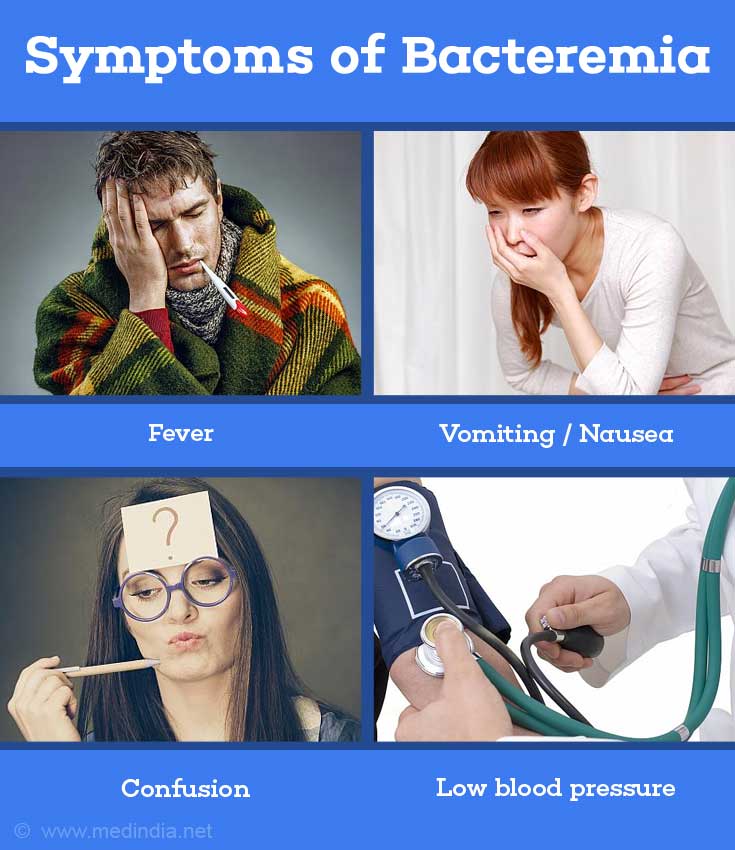
What are the Symptoms of Bacteremia?
The common signs and symptoms of bacteremia are:
- Low blood pressure (hypotension)
- Chills
Fever (> 38°C or <36°C in sepsis).- Increased pulse rate
- Increased respiratory rate
Nausea, vomiting and diarrhea - Confusion
How Do You Diagnose Bacteremia?
It is not easy to diagnose bacteremia. Having said this, the diagnosis of bacteremia is based on the classification of bacteremia. The diagnosis regimen involves microbiological, laboratory, and imaging techniques.(4✔ ✔Trusted Source
Age-related Differences in Symptoms, Diagnosis and Prognosis of Bacteremia.
Go to source)
Blood cultures are used to detect the presence of bacteria in the blood. At least 10 to 20 ml of blood is required. However, what is observed is that bacteria may not always be circulating in the blood and may actually end up in a distant tissue site. The current estimate of positive bacteremia diagnoses puts it at a measly 20%. In a 2009 study, it was observed that when 2 blood cultures were taken in the space of 24 hours, then approximately 90% of bacteremia cases were detected. If 4 blood cultures are performed, then 99% of bacteremia cases are detected.

In the case of secondary bacteremia, the source of infection is at a site away from the blood. Hence, samples from different parts of the body need to be analyzed to find the source of infection. The samples include:
- Wound culture
- Cerebrospinal fluid (CSF) analysis
- Urine analysis and culture
- Pleural fluid culture
- Stool culture
Bone marrow aspiration and culture
Laboratory tests might show the following:
- Elevated procalcitonin levels (a precursor of the hormone calcitonin)
- Elevated white cell counts (leucocytosis) with increased numbers of neutrophils (neutrophilia)
- Elevated ESR (erythrocytic sedimentation rate)
- Elevated C-reactive protein levels
Imaging – The routinely used imaging study is chest x-ray, especially in infants and children to look for pneumonia. Pneumonia should be considered when there is no other source of infection found
Bacteremia that is the result of intravascular devices, such as a catheter, may be effectively diagnosed with paired blood cultures that quantitate the microbiological pathogens. Similarly, acridine orange leukocyte cytospin or catheter-segment culture, are effective in diagnosing intravascular device-related bacteremia. A blood culture from a central venous catheter is more effective than obtaining a blood culture sample from peripheral blood.(5✔ ✔Trusted Source
The Clinical Importance of Microbiological Findings in the Diagnosis and Management of Bloodstream Infections.
Go to source)
How is Bacteremia Treated?
Antibiotic therapy is the standard treatment for bacterial infections. However, there is no clear guideline on the duration of antibiotic administration. Undue long duration of antibiotic treatment can lead to resistance in the bacterial strains as observed in methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE).

It is suggested from a review of clinical studies that a short duration of 5 days to a week of antibiotic treatment may suffice to cure bacterial infections.(6✔ ✔Trusted Source
Staphylococcus Aureus Bloodstream Infections: Definitions and Treatment.
Go to source, 7✔ ✔Trusted Source
Duration of Antibiotic Therapy for Bacteremia: A Systematic Review and Meta-Analysis.
Go to source)
The treatment regimen is decided based on the type of bacteria involved in the infection.
In gram-positive bacteria, there are methicillin-resistant Staphylococcus epidermis and Staphylococcus aureus strains. Vancomycin is used to treat MRSA though some resistance has been noticed. Daptomycin is used to treat bacteremia due to methicillin-sensitive Staphylococcus aureus (MSSA) and methicillin-resistant Staphylococcus aureus (MRSA). Cefazolin and flucloxacillin are other drugs to treat MSSA infections. Similarly, there are vancomycin-resistant Enterococci (VRE). VRE strains may be treated with chloramphenicol, rifampin, tetracycline, quinupristine-dalfopristine, and methicillin.(8✔ ✔Trusted Source
Staphylococcus Aureus Bacteremia: Epidemiology, Pathophysiology, and Management Strategies.
Go to source)
Mortality is high in gram-negative bacterial infections. The drugs used to treat such infections are quinolones, trimethoprim-sulfamethoxazole, b-lactam medications (e.g. acyl ampicillin, carbapenem, 3rd generation cephalosporin), and dual agent therapy with aminoglycosides.
Dual-agent therapy (b-lactam medication with an aminoglycoside) is normally used where the bacteria are resistant to many drugs (e.g. Xanthomonas, Pseudomonas, Aeromonas).
How is Bacteremia Prevented?
Bacterial infections are diverse and so the prevention methods also vary depending on the type of infection.
- Practice good hygiene, such as washing hands and handling body secretions in an appropriate way.
- Maintaining good control of diabetes.
- Infected patients should be isolated to prevent the spread of infection.
- Prompt diagnosis and treatment of primary foci of infections such as urinary tract infections or skin infections.
- The pneumococcal vaccine is 80% effective in preventing mortality due to pneumonia. The vaccine is also 75% effective in reducing the risk of bacteremia in individuals over the age of 65 with a good immune system.
- Hib vaccination in children has reduced the incidence of invasive Hemophilus influenzae disease.