- What is antibiotic resistance? - (https://www.cedars-sinai.org/health-library/diseases-and-conditions/a/antibiotic-resistance.html)
- About Antibiotic Resistance - (https://www.cdc.gov/drugresistance/about.html#:~:text=Antibiotic%20resistance%20happens%20when%20germs,and%20sometimes%20impossible%2C%20to%20treat.)
- Antibiotic resistance - (https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance)
- More Information about Antibiotic Resistance - (https://medlineplus.gov/antibioticresistance.html)
- Antibiotic resistant bacteria - (https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/antibiotic-resistant-bacteria#bacteria-resistant-to-antibiotics)
- Combating Antibiotic Resistance - (https://www.fda.gov/consumers/consumer-updates/combating-antibiotic-resistance)
- Mark Laws, Ali Shaaban, KhondakerMiraz Rahman, Antibiotic resistance breakers: current approaches and future directions, FEMS Microbiology Reviews, Volume 43, Issue 5, September 2019, Pages 490–516 - (https://doi.org/10.1093/femsre/fuz014)
- Ouwehand AC, Forssten S, Hibberd AA, Lyra A, Stahl B. Probiotic approach to prevent antibiotic resistance. Ann Med. 2016;48(4):246-55 - (doi: 10.3109/07853890.2016.1161232. Epub 2016 Mar 26. PMID: 27092975.)
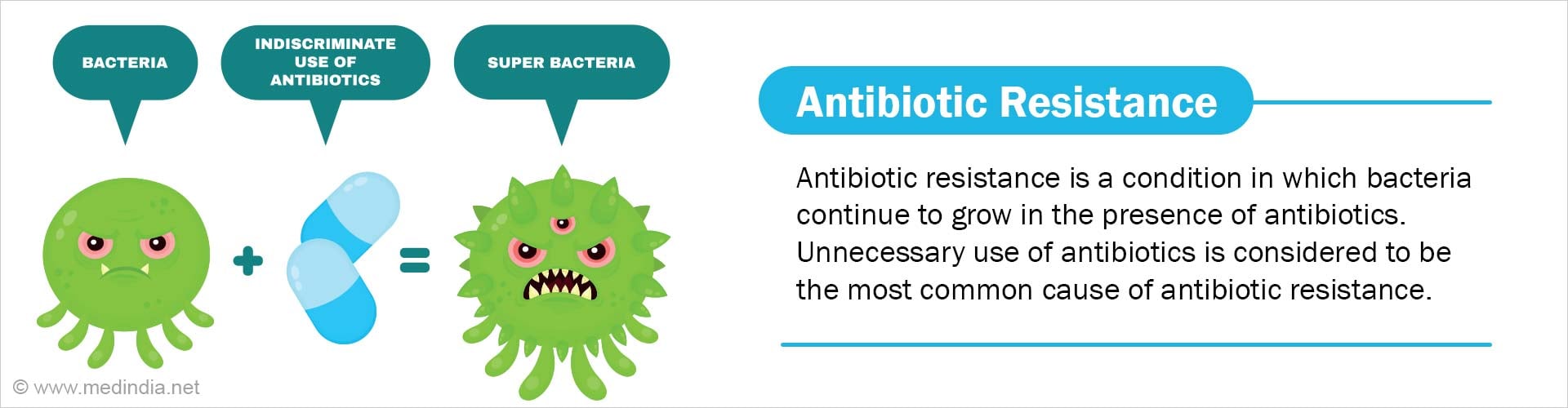
What is Antibiotic Resistance?
Antibiotics are medications used to prevent and treat bacterial infections. They work by destroying bacteria, which can cause illness and disease.
Over time, some bacteria tend to change in such a way that antibiotics cannot eliminate them. As a result, they continue to grow, combating the action of antibiotics.
This condition is referred to as antibiotic resistance, and the infections caused by these types of antibiotic-resistant microbes are called "Antibiotic resistant infections."
How Do Bacteria Do This?
Bacteria make use of multiple defense strategies to become resistant to antibiotics. The most well-known approaches include,
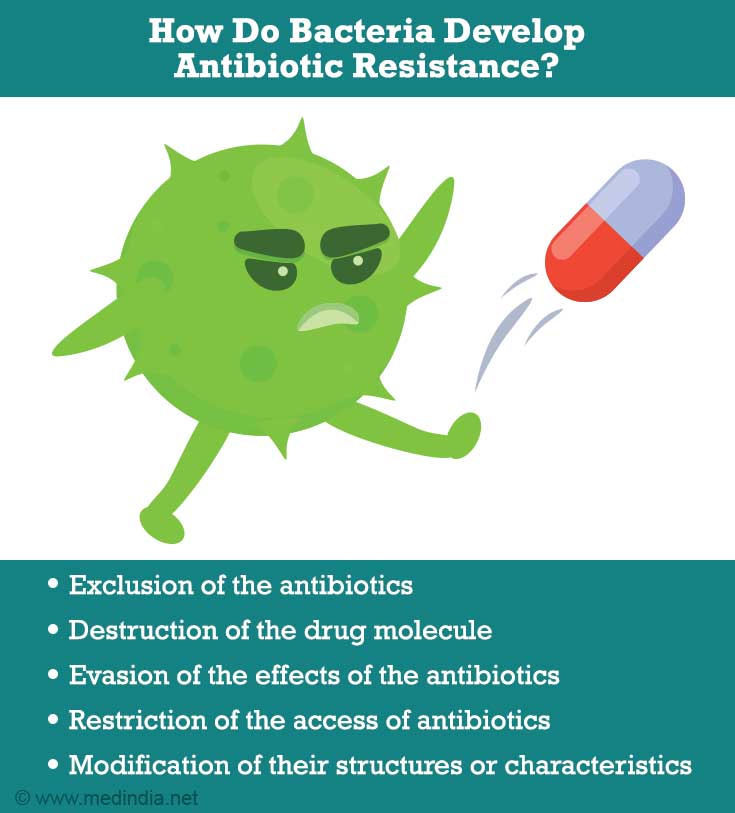
- Exclusion of the antibiotics using pumps in their cell walls
- Destruction of the drug molecule using some unique kinds of proteins
- Evasion of the effects of the antibiotic by developing new cell processes
- Restriction of the access of antibioticsby limiting the number of entry points through which the medications enter into them
- Modification of their structures or characteristics so the drug can no longer fit and do its job
Whenever bacterial infections are treated with antibiotics, there arises a chance for antibiotic resistance. Usually, the medicine kills most of the bacteria, but a small group may survive.
Antibiotic resistance is often linked to a specific bacteria and antibiotic like
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Vancomycin-resistant Enterococcus (VRE)
- Multi-drug-resistant Mycobacterium tuberculosis (MDR-TB)
- Carbapenem-resistant Enterobacteriaceae (CRE) gut bacteria
Unnecessary usage of antibiotics is considered to be the most common cause of antibiotic resistance.
Where Does This Happen?
Bacteria achieve antibiotic resistance across various settings such as,
- Hospitals
- Communities
- Animals carrying antibiotic-resistant bacteria in their gut which could cross over to human beings
New forms of antibiotic-resistant bacteria are emerging and spreading with remarkable speed across continents - making it a global crisis.
Why Does Antibiotic Resistance Matter?
In recent times, many infections such as pneumonia, tuberculosis, blood poisoning, gonorrhea, and foodborne diseases are becoming harder, and sometimes impossible, to treat as the bacteria that cause them have become more resistant to antibiotics.
Since the beginning of the second wave of COVID-19, hospitals have faced multiple issues like a higher number of sick patients to care for and staffing shortages. These issues made it difficult to implement infection control practices in healthcare settings. Experts have raised their concerns as it can create a storm for antibiotic-resistant infections in healthcare settings.
As a result of the shift of focus to the pandemic, public health personnel also experienced difficulties in monitoring antibiotic resistance among the other bacterial strains such as bacteria that cause gonorrhea and food poisoning.
How Are Antibiotic-resistant Infections Treated?
Antibiotic-resistant infections are treated with customized antibiotic treatment regimen based on the type of infection, severity of the disease, and treatment history.
Here’s a list of drugs currently used to treat some of the antibiotic-resistant infections:
|
Name of the Antibiotic-resistant bacterium/ bacterial family |
Currently available treatment options |
|
Methicillin-resistant Staphylococcus aureus (MRSA) |
For moderate infections:
For complicated infections:
|
|
Vancomycin-intermediate and Vancomycin-resistant Staphylococcus aureus (VRSA and VISA) |
|
|
Carbapenem-Resistant Enterobacteriaceae (CRE) |
Avibactam and ceftazidime (Avycaz) Meropenemand vaborbactam (Vabomere) Fosfomycin (Particularly for Urinary Tract Infections) |
|
Vancomycin-resistant Enterococcus (VRE) |
Ampicillin Ampicillin-sulbactam Gentamicin Streptomycin Ceftriaxone Linezolid Daptomycin |
|
Multi-drug-resistant Mycobacterium tuberculosis (MDR-TB) |
|
What Can You Do To Prevent Antimicrobial Illness?
Here are ten ways to combat antibiotic resistance at an individual level.
- Medical professionals should follow standard guidelines when treating infections
- Medical professionals should not use antibiotics unnecessarily
- Medical professionals should give the shortest course of antibiotics as recommended
- Medical professionals should select the commonest antibiotic to treat infections rather than selecting higher antibiotics

- Patients should complete the entire course of the antibiotics as prescribed by your doctor, even if you are feeling better
- Patients should not stop and start antibiotics on your own
- Patients should not take antibiotics prescribed for someone else's illness
- Patients should not stock antibiotics for the next time you get sick
- Patients should avoid taking antibiotics unnecessarily like to treat viral infections such as cold and flu
- Patients should discuss with health care professional if they experience any side effects