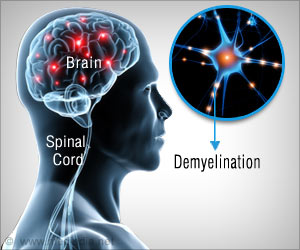
‘Multiple sclerosis patients are three to six times more likely to develop seizures. Using a mouse model, researchers have revealed that chronic demyelination is closely linked to, and is likely the cause of, the seizures.’
Tweet it Now
As though this were not enough, MS patients are three to six times
more likely to develop seizures - abnormal hyperactivity of nerve cells - compared to the rest of the population. However, despite increased
occurrence of seizures among MS patients, little research has been done
to probe why they happen.Using a mouse model, a team of scientists at the University of California, Riverside has found for the first time that chronic demyelination is closely linked to, and is likely the cause of, these seizures. Reporting in the journal Neuroscience, the researchers also note that certain neurons in the brain, called "parvalbumin interneurons," which are important for keeping hyperactivity down, are modified and lost when extensive demyelination occurs in the brain's cortex and hippocampus.
An image from their research is featured on the cover of volume 346 (pages 409-422) of the journal.
"Demyelination causes damage to axons and neuronal loss, specifically parvalbumin interneurons are lost in mice, hyperactivity is no longer down but up, and this could be a cause of seizures," said Seema Tiwari-Woodruff, an associate professor of biomedical sciences in the UC Riverside School of Medicine, whose laboratory authored the research. "It's very likely this is what is occurring in those patients with MS who are experiencing seizures."
In the lab, Tiwari-Woodruff and her team induced demyelination in mice by feeding them a diet that contained cuprizone, a copper-binding substance that causes damage to oligodendrocytes -the brain cells that produce myelin. After nine weeks of feeding them cuprizone, the majority of mice started having seizures.
Advertisement
In another study, after nine or twelve weeks, the researchers stopped feeding the mice the cuprizone diet. Oligodendrocytes began to repopulate the demyelinated areas and remyelinate the intact but myelin-stripped axons. Future studies will assess seizure activity with remyelination.
Advertisement
Her team was recently awarded a pilot grant from the National Multiple Sclerosis Society to compare postmortem brain tissue from MS patients with seizures to those without to understand the cellular basis of seizures in MS. Their findings will also be used to check how well the cuprizone mouse model reproduces the changes seen in humans.
"We want to know if these tissues show what we are seeing in our mouse model," Tiwari-Woodruff said. "Our preliminary data in postmortem tissue show considerable similarity between the two. We now have a mouse model with which we can work to test and suggest some therapeutic cures. When developed, such drugs, which would be aimed at reducing hyperactivity to reduce the incidence of seizures, could also be extended to epilepsy patients."
Source-Eurekalert