‘The nutritional support provided to pregnant women might avoid the risk of environmentally-determined cleft palate and cleft lip but not genetically-determined risk.’
Tweet it Now
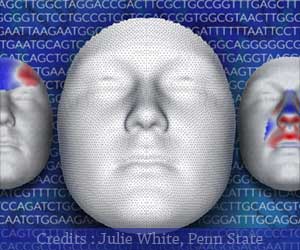
Plastic and reconstructive surgeons are key members of the team of specialists providing care for children with cleft lip and cleft palate, which is one of the most common congenital anomalies.The effect of SES on environmentally versus genetically determined' clefts differs.
Researchers analyzed data from a US nationwide birth database, including approximately 6.25 million births in 2016 and 2017. Of these, 2,984 births (0.05 percent) were affected by CLP and 1,180 by CPO (0.02 percent).
The study examined several proxies for SES, including mother's level of education, use of the federal WIC program (Special Supplemental Nutrition Program for Women, Infants, and Children), and insurance status (Medicaid versus private insurance).
These potential socioeconomic risk factors for CLP or CPO were analyzed with adjustment for other variables, including demographic factors, prenatal care, maternal health, and infant characteristics.
Advertisement
In contrast, receiving WIC assistance was associated with a 25 percent increase in the risk of CPO. In adjusted analyses, Medicaid coverage was unrelated to the risk of CLP or CPO.
Advertisement
In contrast, the timing of prenatal care was unrelated to the risk of CPO.
The study confirmed some previously known risk factors for orofacial clefts. Male sex, first-trimester smoking, and maternal gestational diabetes were all associated with an increased risk of CLP.
Smoking and maternal infections before pregnancy was associated with an increased risk of CPO, while female sex was a protective factor against CPO.
As in previous studies, most risk factors for CPO did not overlap with those for CLP – supporting the theory that these two categories of clefts have different causative factors.
Researchers speculate on some ways that socioeconomic factors might affect the risks of orofacial clefts. For example, mothers with higher education levels might be better informed about and have better access to, prenatal care and adequate nutrition during pregnancy.
Researchers hope their findings will help to clarify the previous mixed results on the relationship between SES and orofacial clefts.
They call for further studies to elucidate the mechanisms underlying the relationship between SES and risks of CLP and CPO to improve and implement public health policies aimed at reducing the burden of clefts and its disproportionate impact on socioeconomically disadvantaged populations.
Source-Medindia