A recent research has found that the cox-2 inhibitor celecoxib, a common pain reliever used to treat arthritis, may reduce the risk of the most common cause of brain damage in premature babies.
The work involves shoring up blood vessels in a part of the brain that in premature infants is very delicate and susceptible to dangerous bleeding, which has an effect on an approximate 12,000 children a year, leaving many everlastingly affected by cerebral palsy, mental retardation, and seizures."Stabilizing the blood vessels right before the baby is born is a tremendous opportunity to save the baby from potentially lifelong complications," said Maiken Nedergaard, M.D., Ph.D., a neuroscientist at the University of Rochester Medical Center who is presenting the results at a neuroscience meeting, Brain '07, in Osaka, Japan May 20-23.
The laboratory research was done principally in a laboratory at New York Medical College led by neonatologist Praveen Ballabh, M.D.
The research is based on extensive brain studies of infants who died prematurely as well as on findings with newborn rabbits, whose brains bear a resemblance to those of premature babies in some very significant ways. The medication would need to be tested thoroughly in pregnant women before being considered as a treatment for their babies. But the investigators indicate that celecoxib is already used widely in people, including pregnant women, making a clinical trial in people possible.
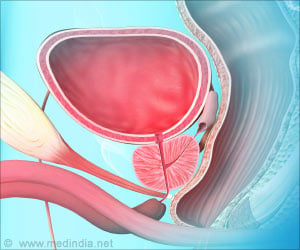
The researchers focused on a part of the brain known in budding infants as the germinal matrix, a temporary formation that is the origin of all brain cells in a baby. The structure runs like an uneven coastline just below spaces in the brain called ventricles, and in premature infants it's enormously active, manufacturing new brain cells that wander and settle into other parts of the brain.
"This is a very, very important part of the brain, from which neurons and glia cells migrate out to form all the layers of the brain," said Ballabh, an associate professor in the Department of Pediatrics, Cell Biology, and Anatomy at New York Medical College, and a neonatologist at Westchester Medical Center.
Advertisement
Babies most at risk are those born between 24 and 32 weeks gestation that weigh less than 1500 grams, or about 3 lbs., 5 ounces. About 20 percent of such infants have a bleed, known as a germinal matrix hemorrhage or an intraventricular hemorrhage. While the problem sometimes is very small and hardly perceptible, other times the bleed causes tremendous brain damage.
Advertisement
The goal was to make the germinal matrix a little hardier in cases of premature birth, by eradicating the vigorous building of new, but very delicate, blood vessels that bleed more easily than established blood vessels. The team used celecoxib to hit down the production of cox-2, which consecutively slowed production of VEGF. The team also studied an anti-cancer drug known as ZD6474, which affects another molecule, angiopoietin-2, that the body uses to build blood vessels.
The team found that in human brain tissue, the compounds significantly abridged the production of cells used to build blood vessels, and decreased levels of angiopoietin-2 and VEGF, the two molecules very active in building new blood vessels.
Results were spectacular in female rabbits that were given the drugs for two days before delivering their offspring prematurely. The team showed that celecoxib cut the risk in offspring of having a moderate or severe bleed in half, from 90 percent to 45 percent. The percentage was reduced even more when ZD6474 was used as well, from 45 to 27 percent, but Nedergaard and Ballabh indicate that ZD6474 is a very powerful medication not likely to be given to pregnant women in the near future.
On the whole, the best way to thwart the problem, doctors say, is to do everything possible to allow a pregnant woman to bear a pregnancy for a full 40 weeks. So doctors put a great deal of effort into preventing preterm labor. But when premature labor can't be prevented, doctors do have a few tools at their disposal to try and prevent bleeds in the germinal matrix.
"This work is very exciting, but the work is ongoing, and we must investigate the use of celecoxib more thoroughly before considering it for widespread use to prevent this problem," said Ballabh. "We can fix many problems in the premature infant, but brain damage is one problem that cannot be fixed – it must be prevented. Right now there is nothing available that has been shown to be really effective at preventing this problem."
Source-ANI
SRM/B