Under some health plans, HIV drugs may cost a patient nearly $3,000 more per year than in other plans, said the study led by Harvard University.
"Eliminating discrimination on the basis of preexisting conditions is one of the central features of the Affordable Care Act (ACA)," said lead author Doug Jacobs of the Harvard T.H. Chan School of Public Health.
"However, the use of formularies to increase costs and dissuade those with preexisting conditions such as HIV from enrolling in the plan threatens to at least partially undermine this goal of the ACA."
The practice that Jacobs and his colleagues identified is called "adverse tiering," in which all drugs for certain conditions are placed in the highest cost-sharing tiers.
Advertisement
Six of the states analyzed were mentioned in a legal complaint to the Department of Health and Human Services for alleged adverse-tiering: Delaware, Florida, Louisiana, Michigan, South Carolina and Utah.
Advertisement
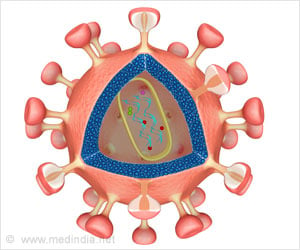
About one quarter of the plans examined used discriminatory drug tiering for one of the most common classes of HIV medications, known as nucleoside reverse-transcriptase inhibitors (NRTIs).
"We found evidence of adverse tiering in 12 of the 48 plans and 7 of the 24 plans in the states with insurers listed in the HHS complaint and 5 of the 24 plans in the other six states," said the study.
"Our findings suggest that many insurers may be using benefit design to dissuade sicker people from choosing their plans."
People who enrolled in adverse-tiering plans (ATPs) paid on average three times more for HIV medications than people in non-ATP plans, with a nearly $2,000 annual difference even for generic drugs, according to the study.
Despite the generally lower annual premiums associated with adverse-tiered plans, customers with HIV paid an average of $3,000 more for treatment per year than they would have under a non-ATP plan.
The researchers warned that the practice could put significant financial strain on ill people and could "lead to sicker people clustering in plans that offer more generous prescription drug benefits -- which could in turn create a 'race to the bottom' in insurers' drug plan designs as they try to avoid a large influx of sick enrolees that would negatively affect profits."
Source-AFP