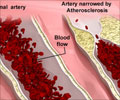
Lurking within our arterial walls are immune system cells called macrophages (Greek for "big eater") whose essential function is to consume other cells or matter identified as foreign or dangerous. "When they do that, it means they consume the other cell''s store of cholesterol," said Christopher Glass, MD, PhD, a professor in the Departments of Medicine and Cellular and Molecular Medicine and senior author of the Cell study. "As a result, they''ve developed very effective ways to metabolize the excess cholesterol and get rid of it."
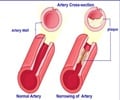
But some macrophages fail to properly dispose of the excess cholesterol, allowing it to instead accumulate inside them as foamy lipid (fat) droplets, which gives the cells their particular name: macrophage foam cells.
These foam macrophages produce molecules that summon other immune cells and release molecules, signaling certain genes to launch an inflammatory response. Glass said conventional wisdom has long assumed atherosclerotic lesions - clumps of fat-laden foam cells massed within arterial walls - were the unhealthy consequence of an escalating association between unregulated cholesterol accumulation and inflammation.
Glass and colleagues wanted to know exactly how cholesterol accumulation led to inflammation, and why the macrophages failed to do their job. Using specialized mouse models that produced abundant macrophage foam cells, they made two unexpected discoveries that upend previous assumptions about how lesions form and how atherosclerosis might be more effectively treated.
"The first is that foam cell formation suppressed activation of genes that promote inflammation. That''s exactly the opposite of what we thought happened," said Glass. "Second, we identified a molecule that helps normal macrophages manage cholesterol balance. When it''s in abundance, it turns on cellular pathways to get rid of cholesterol and turns off pathways for producing more cholesterol."
Advertisement
"That''s the next thing to study; why that happens," Glass said, hypothesizing that the cause may be linked to overwhelming, pro-inflammatory signals coming from proteins called Toll-like receptors on macrophages and other cells that, like macrophages, are critical elements of the immune system.
Advertisement
Glass noted that a synthetic molecule similar to desmosterol already exists, offering an immediate test-case for new studies. In addition, scientists in the 1950s developed a drug called triparanol that inhibited cholesterol production, effectively boosting desmosterol levels. The drug was sold as a heart disease medication, but later discovered to cause severe side effects, including blindness from an unusual form of cataracts. It was pulled from the market and abandoned.
"We''ve learned a lot in 50 years," said Glass. "Maybe there''s a way now to create a new drug that mimics the cholesterol inhibition without the side effects."
Co-authors are first author Nathanael J. Spann, Norihito Shibata, Donna Reichart, Jesse N. Fox and Daniel Heudobler, UCSD Department of Cellular and Molecular Medicine; Lana X. Garmire, UCSD Department of Bioengineering; Jeffrey G. McDonald and David W. Russell, Department of Molecular Genetics, UT Southwestern Medical Center; David S. Myers, Stephen B. Milne and Alex Brown, Department of Pharmacology, Vanderbilt Institute of Chemical Biology; Iftach Shaked and Klaus Ley, La Jolla Institute of Allergy and Immunology; Christian R.H. Raetz, Department of Biochemistry, Duke University School of Medicine; Elaine W. Wang, Samuel L. Kelly, M. Cameron Sullards and Alfred H. Merrill, Jr., Schools of Biology, Chemistry and Biochemistry and the Parker H. Petit Institute of Bioengineering and Bioscience, George Institute of Technology; Edward A. Dennis, UCSD Department of Chemistry and Biochemistry; Andrew C. Li, Sotirios Tsimikas and Oswald Quehenberger, UCSD Department of Medicine; Eoin Fahy, UCSD Department of Bioengineering; and Shankar Subramaniam, UCSD Departments of Cellular and Molecular Medicine, Bioengineering and Chemistry and Biochemistry.
Funding for this research came, in part, from National Institutes of Health grants GM U54069338 (to the LIPID MAPS Consortium), P01 HC088093 and P01 DK074868.
###
Source-Newswise