“Anal cancer was widely associated with HIV-infected men who have sex with men,” said Mark H. Einstein, MD, MS, Director of Clinical Research, Division of Gynecologic Oncology at Montefiore Medical Center and Professor at Albert Einstein College of Medicine. “But now, this study reveals anal precancerous disease in a high proportion of women with HIV.”
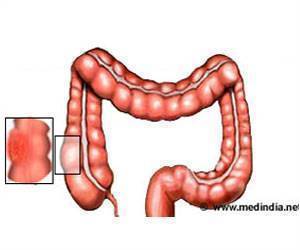
Out of 715 asymptomatic HIV-infected women studied, 10.5% exhibited some form of anal disease and approximately one third of them were found to be true pre-cancerous disease. The researchers determined that this is likely due to the fact that HIV promotes human papillomavirus (HPV) persistence and consequently, which is known to cause nearly all anal cancers. HIV-infected individuals are also at increased risk for the development of many other HPV-associated neoplasms.
The incidence of anal carcinoma (AC) has been increasing despite the implementation of antiretroviral therapy (ART), which has not been shown to consistently alter the course of HPV–associated anogenital disease.
The women studied were Montefiore patients in the Bronx, which has one of the highest HIV prevalence rates in the United States. Data indicates that 1.8% of the Bronx population is known to be HIV infected, representing 3% of the total number of HIV patients in the entire country. Montefiore is the largest provider of medical services for people with HIV in the Bronx and has adopted routine screening for AC with annual anal cytology in all HIV-infected patients.
As a result of these findings, Dr. Einstein and his colleagues recommend that all HIV+ women who have any abnormal anal cytology be referred for high resolution anoscopy, particularly those with poorly controlled HIV who are significantly at even higher risk for harboring a high-grade AIN than women who are well controlled. Also, all HIV infected men and women should be considered for anal cancer screening. Given the lower high-grade anal disease prevalence in women with well-controlled HIV, other strategies to improve disease ascertainment, such as inclusion of HPV testing might be found to be useful for AC screening. This risk stratification might prove to be different for women than it is for men, where prevalence rates seem to be considerably higher. Given the high rate of high-grade anal precancerous lesions in screened HIV-infected women and an aging population of HIV-infected patients, measures to increase routine AC screening should be strongly considered. Depending on the size of the pre-cancerous legion, it can be removed long before it becomes cancer, thus being able to save lives.
Advertisement
Dr. Einstein’s primary research interests focus on the pathogenesis and therapy for cervical cancer. He has developed and has been leading numerous multi-institutional clinical trials in targeting HPV and cervical cancer as well as cervical cancer prevention. He is active in clinical trial cooperative groups as Co-Chair of the Gynecologic Oncology Group Vaccine Committee and sits on the GOG Cervix Committee. He is on the HPV working group of the NCI Aids Malignancy Consortium. Dr. Einstein is also a program leader of the Gynecology Division of the New York Cancer Consortium and is the primary investigator of many of its gynecologic cancer therapeutics trials accruing patients throughout New York hospitals. He is active in policy-making regarding cervical cancer prevention, participating in the development of the American Cancer Society recommendations for HPV vaccines as well as the working group for the Society of Gynecologic Oncology’s (SGO) HPV vaccine recommendations. He is Chair of the Gynecologic Oncology Foundation’s (GCF) National Cervical Cancer Public Education Campaign and sits on their Board of Directors.
Advertisement