‘Stem cell transplants seem no better than conventional therapy for Crohn's disease, says study.’
Tweet it Now
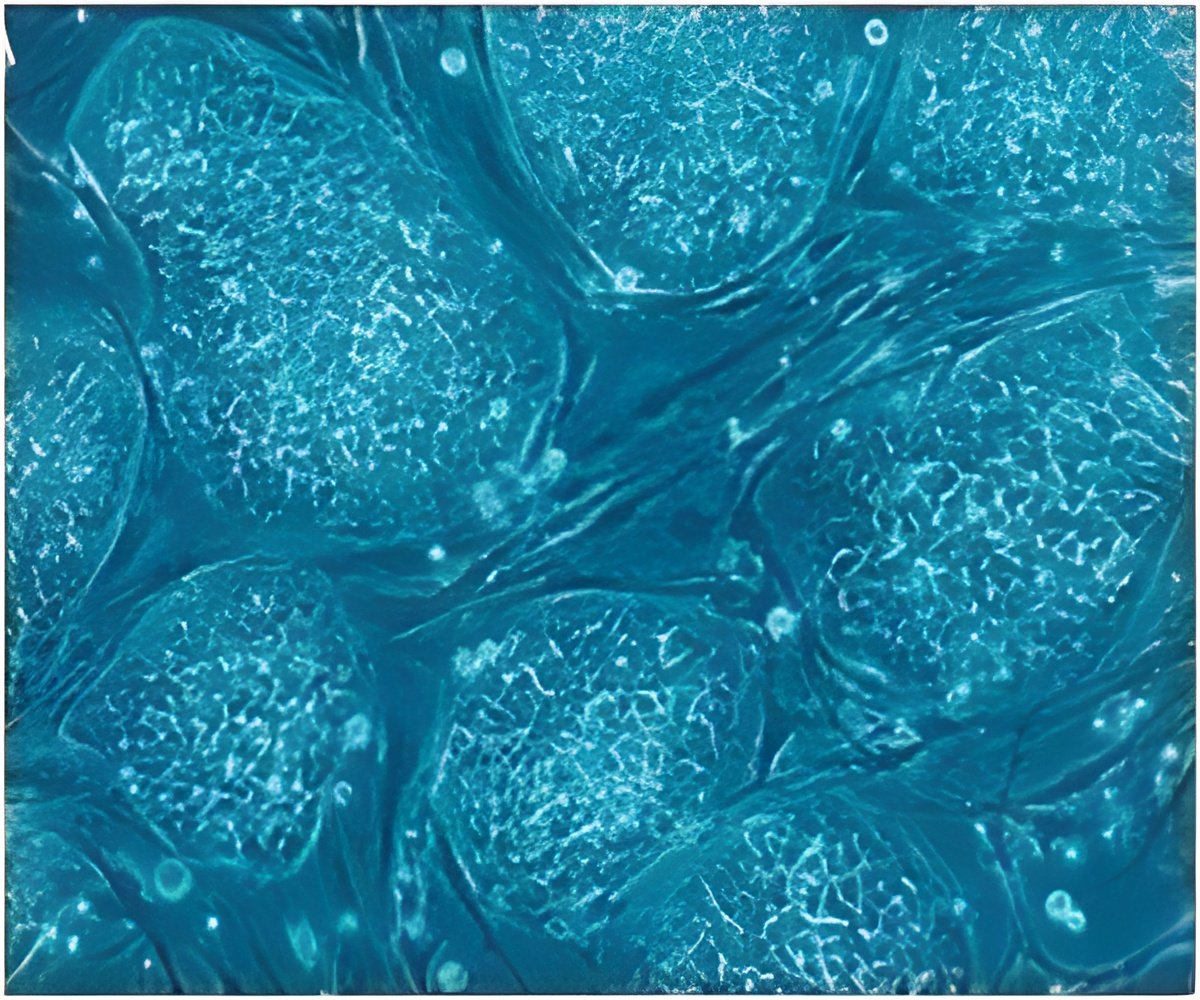
Patient case reports had suggested that blood stem cell transplantation (HSCT) may help some patients so an international randomised clinical trial was set up by the Nottingham Digestive Diseases Centre (NDDC) to test this hypothesis. The results are published in the Journal of the American Medical Association. The researchers randomly assigned 45 patients with Crohn's disease who were not responsive to treatment or suitable for surgery to autologous (the use of one's own cells) blood stem cell treatment or a control treatment in groups of 23 and 22. Patients were aged between 18 and 50 years and all were given standard Crohn's treatment as needed. The trial involved 11 European transplant units from July 2007 to September 2011 with follow-up until March 2013.
Leading the trial, Professor Chris Hawkey of the Nottingham Digestive Diseases Centre, said: "We found there was no statistically significant difference between the groups in the proportion of patients who met our highly stringent definition of sustained disease remission after treatment -- only two in the stem cell transplant group (8.7 percent) and one in the control group (4.5 percent). However, there was a significant difference among patients able to discontinue active treatment in the last three months of participation in the trial -- 61 percent in the stem cell group and 23 per cent in the control, and objective signs of disease disappeared in about a quarter of patients.
"There were 76 serious adverse events in patients undergoing stem cell therapy and 38 in the control group. Because very few patients achieved sustained disease remission, we conclude that HSCT is unlikely to alter the natural history of Crohn disease, and our findings argue against extension of HSCT to a wider group of patients outside of future additional trials."
Professor Dominique Farge Bancel, Saint Louis Hospital in Paris and Chair of the European Blood and Marrow Transplantation Society, added: "Although autologous HSCT therapy showed more toxicity in early stages of the follow-up in Crohn's patients, long term results after HSCT treatment may shed new lights on the expected benefit, as observed in Scleroderma, another autoimmune disease where the proof of a HSCT superiority over conventional therapy was obtained only after long term follow-up at the price of higher early toxicity."
Advertisement
Advertisement