"The amniotic membrane is medical waste that could be collected and used after delivery," said Dr. Shunichiro Miyoshi, co-author of the study and assistant professor in the cardiology department and Institute for Advanced Cardiac Therapeutics at the Keio University School of Medicine in Tokyo.
In laboratory studies, the hAMCs transformed into heart muscle cells, and 33 percent of them were beating spontaneously.
They improved function of rat hearts 34 percent to 39 percent when injected two weeks after a heart attack, while untreated hearts continued to decline in function.
hAMCs decreased the scarred area of damaged rat hearts 13 percent to 18 percent when injected after a heart attack.
They survived for more than four weeks in the rat heart without being rejected by the recipient's immune system, even without immunosuppressive medication.
Advertisement
It is believed that the implanted cells were not rejected because the amniotic sac is a barrier between a woman and her developing fetus.
Advertisement
This means the usual tissue-type matching (HLA typing) needed prior to transplantation would not be needed if hAMCs were used. Drugs to suppress the immune system also might not be needed after transplant.
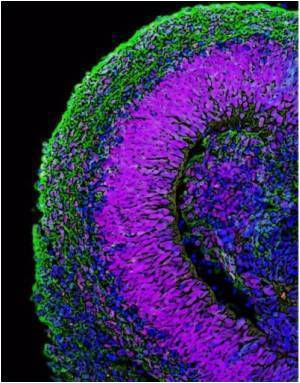
The findings also suggest that hAMCs can differentiate into cells of various organs.
"If we had to create a cell bank system to cover every HLA type, we would need to store a great amount of cells, many of which would never be used. Because hAMCs do not require such a system, it would be less expensive and usable for all patients," said Miyoshi.
Much work remains to be done before testing hAMCs in humans, said the researchers, who are repeating their experiments in larger animals and working to boost the number of heart cells generated y the hAMCs.
The investigators "are to be congratulated for their careful work that has brought forward a cell type that may offer the real potential for off-the-shelf cardiac myocyte [muscle cell]-based therapy," said Dr. Marc S. Penn, and Dr. Maritza E. Mayorga.
The study was published in Circulation Research: Journal of the American Heart Association.
Source-ANI
TAN