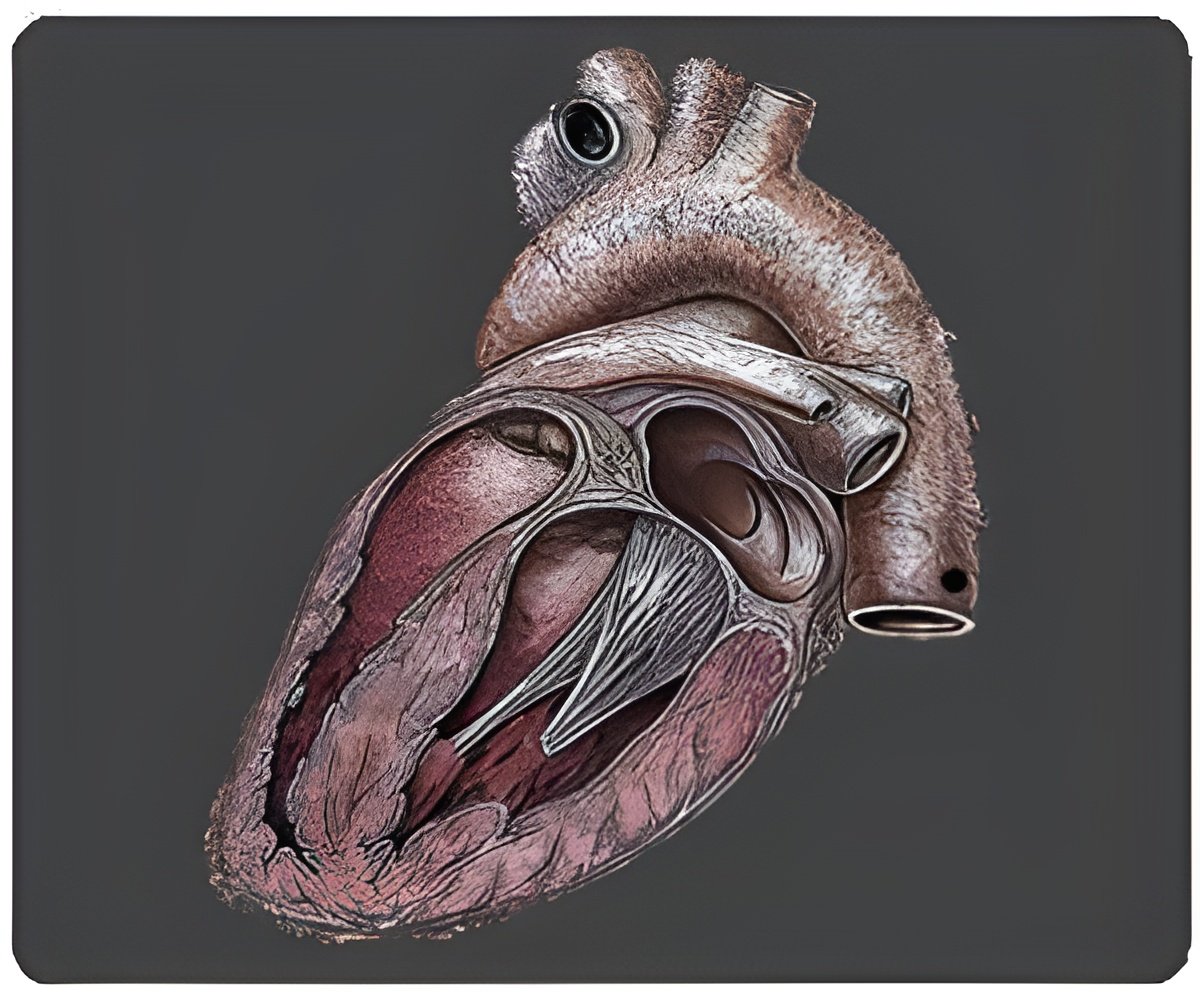
‘Using advanced stem cell technology, scientists from the Icahn School of Medicine at Mount Sinai have created a model of hypertrophic cardiomyopathy (HCM).’
Tweet it Now
The genetic disorder discussed in the new study is called cardiofaciocutaneous syndrome (CFC), which is caused by a mutation in a gene called BRAF. The condition is rare and affects fewer than 300 people worldwide, according to the National Institutes of Health. It causes abnormalities of the head, face, skin, and major muscles, including the heart. To learn more about HCM associated with various genetic diseases, Mount Sinai scientists took skin cells from three CFC patients and turned them into highly versatile stem cells, which were then converted into cells responsible for the beating of the heart. This model has relevance for research on several related and more common genetic disorders, including Noonan syndrome, which is characterized by unusual facial features, short stature, heart defects, and skeletal malformations.
"At present, there is no curative option for HCM in patients with these related genetic conditions," said Bruce D. Gelb, Director of The Mindich Child Health and Development Institute and Professor in the Departments of Pediatrics, Genetics and Genomic Sciences at the Icahn School of Medicine at Mount Sinai. "If our findings are correct, they suggest we might be able to treat HCM by blocking specific cell signals - which is something we know how to do."
Dr. Gelb says that about 40% of patients with CFC suffer from HCM (two of the three study participants had HCM). This suggests a pathogenic connection, though the link has never been fully explored or explained. The primary goal of the current research was to understand the role of a cell-signaling pathway called RAS/MAPK in the cascade of events leading to HCM in patients with CFCs - and by association, with Noonan syndrome, Costello syndrome, and other similar illnesses.
Observing the disease progression in these heart cells, called cardiomyocytes, Dr. Gelb and his team found that some of the changes were caused by interactions with cells that resemble fibroblasts - the same kinds of cells that produce collagen and other proteins. Fibroblasts make up a significant portion of total heart tissue, although it is the cardiomyocytes that are primarily responsible for pumping blood. "These fibroblast-like cells seem to be producing an excess of a protein growth factor called TGF-beta, which, in turn, caused the cardiomyocytes to hypertrophy, or grow larger," Dr. Gelb said. "We believe this is the first time the phenomenon has been observed using a human induced pluripotent stem cell model of the disease."
Advertisement
The therapeutic implications may also be profound. "We were able to block TGF-beta in vitro using antibodies that bind to the protein. When we did that, the cardiomyocytes no longer hypertrophy," Dr. Gelb said. It's not certain the same effect would be seen in the many clinical cases of HCM that are not influenced by BRAF or the RAS pathway - essentially a chain of cellular proteins that help transmit signals from surface receptors on the cell to DNA in the nucleus -but researchers believe this could be the case.
Advertisement
Source-Eurekalert